EDITORIAL
The articles in this issue cover a wide range of topics, including the role of the maternal microbiome in fetal growth restriction, the effectiveness of therapy for mixed vaginitis, management strategies for pregnant women with COVID-19, the impact of environmental factors on reproductive health, thrombotic complications of chemotherapy, the connection between the microbiome and obesity, as well as rare clinical cases. Innovations in diagnostics, treatment, and screening are explored, from non-invasive prenatal testing to mathematical models for studying autism. The articles emphasize the importance of a comprehensive approach and the integration of modern technologies.
ОRIGINAL ARTICLES
What is already known about this subject?
► Late fetal growth retardation (FGR) remains one of the understudied pathologies, and questions related to its pathogenesis, prevention and treatment are still unanswered.
► FGR is a cause for perinatal and adult delayed complications.
What are the new findings?
► Significant associations between gut microbiome in pregnant women and fetal weight at birth were found.
► A regression model for assessing a relationship between newborn birth weight and the percentage of rectal Corio-
bacteriales Coriobacteriaceae Collinsella in pregnant women was constructed.
► It was found that inflammatory diseases of the lower genital tract and manifestation of urinary infection are more frequent at gestational age of 28–32 weeks, which may be a critical period for late FGR development.
How might it impact on clinical practice in the foreseeable future?
► Monitoring and managing inflammatory processes through analysis of the gut microbiome and inflammatory markers may reduce a risk of developing FGR-associated complications.
► Improving the monitoring and prevention of infectious and inflammatory diseases in pregnant women at gestational age of 28–32 weeks may reduce a risk of late FGR development.
► Personalized approach to correct maternal microbiome may become a new direction in prevention and treatment of perinatal complications, which may improve pregnancy outcomes.
Aim: to analyze a rectal microbiome composition in pregnant women and assess its potential impact on developing of idiopathic late fetal growth retardation (FGR) syndrome.
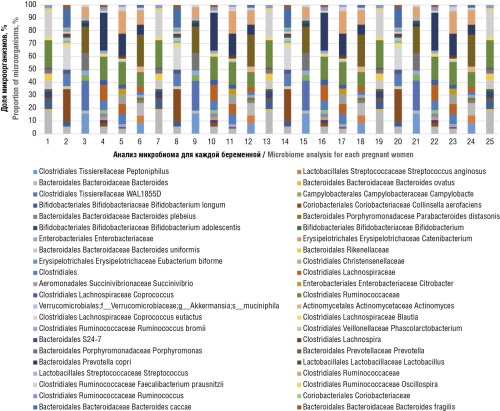
Materials and Methods. We analyzed a course of pregnancy and labour in 80 pregnant women: main group consisted of 40 pregnant women with FGR, control group – of 40 healthy pregnant women. The analysis of the intestinal microbiota in 53 pregnant women (25 pregnant women with late FGR and 28 healthy pregnant women) was carried out by using nitrogenous base sequencing in the 16S ribosomal RNA (rRNA) genes.
Results. Analyses of the gut microbiome composition in pregnant women in study groups revealed significant differences particularly showing a 1.0 % increase in the proportion of Clostridiales Ruminococcaceae Oscillospira that correlated with a 331.7 g increase in neonatal weight gain; a 1.0 % increase in the level of Coriobacteriales Coriobacteriaceae Collinsella was associated with a 476.2 g decrease in neonatal weight gain. The Firmicutes/Bacteroides ratio was 2,0 and 3.6 in main and control group (p = 0.02), respectively, which may suggest about a microbiological dysbiosis with putative pathophysiological outcomes. A significant association between elevated leucocyte counts (in the absence of other manifestations of inflammatory processes) and the probability of FGR development was found. A white blood cell count ≥ 11.05×109/L predicted the risk of FGR with a sensitivity of 60.6 % and a specificity of 79.2 %. Also, erythrocyte sedimentation rate level of ≥ 41.5 mm/hour was associated with increased FGR risk, demonstrating a sensitivity of 85.7 % and specificity of 70.6 %.
Conclusion. It can be concluded that gut dysbiosis may play a role in development of late idiopathic FGR. A negative correlation between a decreased Firmicutes/Bacteroides ratio as well as higher Actinobacteria proportion and fetal birth weight was found.
What is already known about this subject?
► Рathological whites remain one of the most common pathologies with which patients turn to gynecologists during outpatient consultations comprising more than 50 % in pattern of all infectious and inflammatory diseases.
► Researchers recognize the existence of microbial combinations as the main predisposing factors in development of mixed vaginitis.
► Currently, mixed vaginitis frequently adopts a recurrent course, which turns into a chronic inflammatory process. The presence of several microorganisms negatively affects the immune system compared to exposure to a single microorganism, which complicates disease diagnostics and treatment.
What are the new findings?
► The clinical and laboratory parameters assessing effectiveness of mixed vaginitis during combination therapy by Gainomax and Gainomax plus reached 95.6 %. Insufficient therapeutic effectiveness was recorded in 7/158 (4.4 %) women, while normalization of vaginal contents pH value reached 4.1 ± 0.4, Lactobacilli count increased up to 107 ± 2.8 CFU/cm3, eradication of opportunistic bacteria and genus Candida fungi occurred.
► Disease-related symptoms completely regressed in 151/158 (95.6 %) of patients, which significantly increases the odds of clinical recovery.
How might it impact on clinical practice in the foreseeable future?
► A drug course according to the instructions for use is associated with a minimal risk of disease resistance and helps to prevent recurrence of the pathological process.
► Positive aspects such as the lack of any-reason drug withdrawal specified in the informed consent evidence about a high patients’ adherence to therapy and allows the drug to be used in treatment of mixed vaginitis beginning from the first day at the outpatient stage.
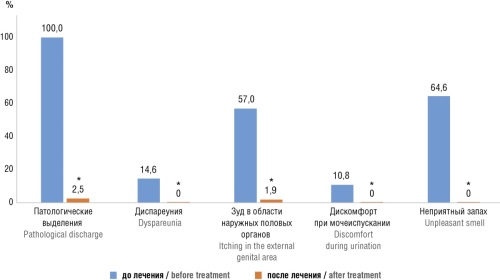
Aim: to assess the effectiveness of combination therapy in reproductive age patients with mixed vaginitis.
Materials and Methods. A retrospective analysis of the therapeutic effectiveness for mixed vaginitis in 158 patients aged 18 to 45 years was carried out. For treatment, the drugs Gainomax (standard dose – thioconazole 100 mg, tinidazole 150 mg in the form of a suppository) and Gainomax plus (standard dose – thioconazole 200 mg, tinidazole 300 mg, lidocaine 100 mg in the form of a suppository) were used for 3 days. The criteria for treatment effectiveness were disappearance of clinical symptoms and normalization of laboratory parameters.
Results. Clinical and laboratory efficacy of therapy reached 95.6 %. Lack of therapeutic effectiveness presented as persistent complaints from patients was recorded in 7 out of 158 (4.4 %) of patients, at the same time, the normalization of vaginal pH was established (pH = 4.1 ± 0.4), the Lactobacilli count increased up to 107 ± 2.8 CFU/cm3, eradication of other opportunistic bacteria and fungi Candida occurred. No side effects were reported while assessing drug safety and tolerability.
Conclusion. Therapy combining thioconazole and tinidazole in treatment of patients with mixed vaginitis demonstrated high effectiveness.
What is already known about this subject?
► Novel coronavirus infection COVID-19 can aggravate pregnancy, leading to perinatal complications.
► Intoxication syndrome plays a leading role in COVID-19 pathogenesis and its severity determines the disease outcome. In most cases, the gastrointestinal tract is the primary site of toxin accumulation.
► Effectiveness of enterosorption in treating preeclampsia and intoxication syndromes of various etiologies has been evidenced.
What are the new findings?
► The efficacy and safety of adding colloidal silicon dioxide to standard treatment for high-risk pregnant women with mode-
rate COVID-19 were evaluated.
► Advanced treatment strategies for high-risk pregnant women with moderate COVID-19 reduce toxic burden by significantly mitigating its negative impact on pregnancy, labor, fetal development, and neonatal outcome.
How might it impact on clinical practice in the foreseeable future?
► These findings suggest a relevance of using colloidal silicon dioxide within a comprehensive treatment regimen for high-risk pregnant women with moderate COVID-19.
► It is worth noting about an indirect beneficial effect related to colloidal silicon dioxide on uteroplacental blood flow that determines pregnancy and delivery outcomes.
Aim: to assess efficacy and safety of using colloidal silicon dioxide as an adjunct therapy in managing high-risk pregnant women with moderate COVID-19.
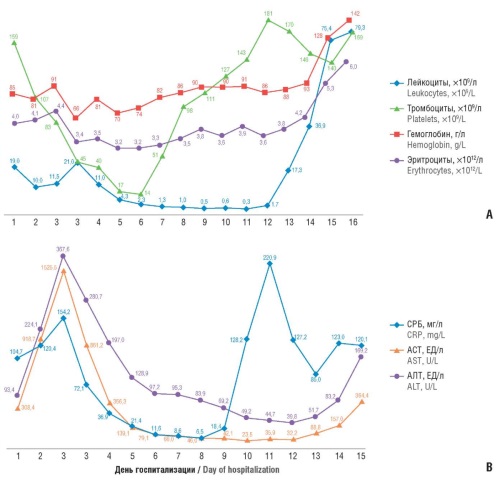
Materials and Methods. A prospective comparative study was conducted by enrolling 62 pregnant women hospitalized with moderate COVID-19. Metabolic charts and delivery records were subsequently reviewed. Participants were divided into two groups: Group 1 (n = 32) received standard treatment, while Group 2 (n = 30) received standard treatment plus colloidal silicon dioxide. Clinical and laboratory markers of endotoxemia, pregnancy progression, and outcomes were assessed.
Results. It was found that in Group 2 vs. Group 1 mean length of the following symptoms was significantly shorter: hyperthermia – by 2.4 days (p = 0.011), tachycardia – by 2.2 days (p = 0.037), weakness – by 2.1 days (p = 0.137), and headache – by 1.7 days (p = 0.042). In addition, women from Group 2 also showed significantly lower C-reactive protein and interleukin-6 levels (p = 0.006 and p = 0.019, respectively) as well as lacked blood flow disturbances at significantly more frequent level primarily Grade 1B uteroplacental insufficiency. Grade III blood flow disturbances were observed in one patient in Group 1 but none in Group 2. Regarding delivery outcomes, 97 % of Group 1 pregnancies resulted in live births (mean body length – 49.25 ± 1.75 cm, mean birth weight – 3126 ± 245.6 g), with vacuum extraction observed in 9 % of cases and cesarean section – in 31 %. One case of antepartum fetal demise occurred. In Group 2, all pregnancies resulted in live births (mean body length – 51.5 ± 2.5 cm, mean birth weight – 3360 ± 260 g), with vacuum extraction in 3 % of cases and cesarean section – in 30 %. While some patients exhibited combinations of these parameters, no significant inter-group differences were found. Assessing neonatal condition at one minute postpartum revealed significantly more cases of mild asphyxia in Group 1; the number of newborns without asphyxia was twice as high in Group 2 (p = 0.021).
Conclusion. Comparing course of pregnancy, delivery, neonatal condition, and management of high-risk pregnant women with moderate COVID-19 using the proposed methodology suggests its high efficacy and safety.
What is already known about this subject?
► Non-invasive prenatal testing (NIPT) for fetal chromosomal abnormalities is one of the most informative and safest methods of prenatal diagnosis. The cell-free fetal DNA (cffDNA) level is the key NIPT quality and accuracy indicator.
► At present, the main trend is to search for anamnestic and clinical factors that may influence the cffDNA level, with the aim to potentiating NIPT diagnostic effectiveness.
► The most effective method for NIPT is the use of various high-throughput sequencing technologies.
What are the new findings?
► Upon using semiconductor sequencing technology the cffDNA level has been shown to depend on the type of blood collection tube, pregnant women age and body mass index, gestational age, early prenatal screening biochemical indicators, fetal trisomy 18.
► The cffDNA level has been shown to increase in pregnant women with fetal congenital defects based on ultrasound data.
► The factors such as the conception type, first-trimester ultrasound early prenatal screening parameters, fetal sex chromosome anomalies, fetal trisomy 13 and 21, or pregnancy complications do not affect cffDNA level.
How might it impact on clinical practice in the foreseeable future?
► The results obtained will expand knowledge about the processes of cffDNA release into the blood plasma in pregnant women, assist in interpreting NIPS data and contribute to improving NIPS methods.
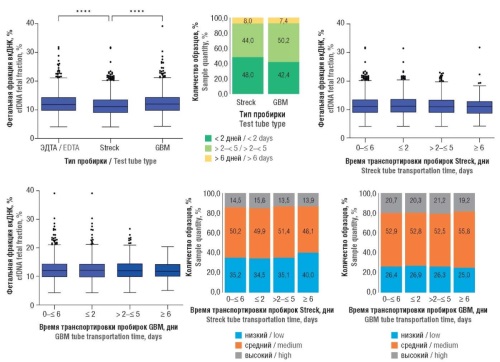
Introduction. Currently, non-invasive prenatal testing (NIPT) is widely used to assess a risk of fetal chromosomal anomalies. NIPТ accuracy depends on the cell-free fetal DNA (cffDNA) percentage relative to total cell-free DNA in the pregnant woman's blood (cfDNA fetal fraction, FF). Despite numerous studies, no consensus regarding FF-affecting factors has been reached yet.
Aim: to investigate a relationship between FF and clinical-anamnestic parameters of pregnant women, pregnancy characteristics, and outcomes using the developed NIPТ technology.
Materials and Methods. A prospective observational study was performed by assessing plasma samples from 5459 women with > 9 week-long singleton pregnancies. NIPТ was performed using semiconductor sequencing followed by bioinformatics data processing, including FF determination, according to a previously developed original algorithm.
Results. Median FF was 11.7 [9.5–14.0] %. It was demonstrated that FF depends on blood collection tube type (p < 0.05). FF was found to decrease with woman age and body mass index, and increase with gestational age, elevated early prenatal screening (EPS) biochemical markers – pregnancy-associated plasma protein-A (РАРР-А) and free beta-subunit of human chorionic gonadotropin (β-hCG) levels (p < 0.05). It has been shown that the FF in pregnant women with trisomy 18 is lower than normal (p < 0.05). An increase in FF was observed in pregnant women with fetal congenital anomalies according to ultrasound results (p < 0.05). No association was found between FF and the conception type, first-trimester ultrasound parameters (nuchal translucency, crown-rump length, ultrasound chromosome anomalies markers), fetal trisomy 13 and 21, fetal sex chromosome anomalies, or pregnancy complications – preeclampsia, gestational diabetes, preterm birth, and fetal growth restriction (p > 0.05).
Conclusion. The identified patterns are important to take into consideration while using and interpreting NIPТ.
REVIEW ARTICLES
What is already known about this subject?
► Chemotherapy (СТ) increases a risk of deep vein thrombosis (DVT) and recurrent DVT by 6- and 2-fold, respectively. Recent studies have proven the role of antitumor СТ in elevating the thrombotic risk in cancer patients.
► Analysis of thrombosis pathogenesis during СТ is complicated by applying various drug combinations and treatment regimens, as well as the inability to fully assess a baseline patient hemostasis state, including the presence of acquired and congenital thrombophilia, etc.
► Despite whole set of data showing that systemic СТ promotes development of venous and arterial thrombosis in cancer patients, no consensus regarding underlying pathogenetic mechanisms has been achieved.
What are the new findings?
► This article analyzes the mechanisms of prothrombogenic action of major currently used СТ drugs. All variants of pathogenetic pathways for enabling such effects are described in detail thereby allowing to model various strategies that counteract thrombosis.
How might it impact on clinical practice in the foreseeable future?
► The prothrombogenic effect of chemotherapy drugs necessitates to consider the issue of simultaneous planning of antithrombotic prophylaxis. A better understanding of the mechanisms that control СТ-associated thrombosis will enable the development of optimal anticoagulant regimens that minimize thrombotic and bleeding risks.
► It is obviously required to develop and implement a prognostic model for thrombosis risk stratification in patients undergoing СТ followed by assessing a need for conducting prophylactic anticoagulation as well as randomized controlled trials on using prophylactic anticoagulation during СТ.
Cancer patients are at risk of developing arterial and venous thrombosis during chemotherapy (CT) and after its cessation. A prothrombotic risk may arise via pathogenetic pathways such as activation of external and internal coagulation pathways, decreased anticoagulant levels, platelet activation, fibrinolysis blockade, etc. Chemotherapeutic agents exert direct cytotoxicity, as well as indirectly suppress cellular processes necessary for tumor cell proliferation. CT-related cytotoxicity act on both tumor and healthy body cells. Available targeted drugs with improved selectivity for tumor cells are also associated with thrombosis risk. Low molecular weight heparins, which effectively reduce the risk of venous thromboembolism, have not yet been officially recommended for routine use during CT. Here, we discuss the prothrombotic effects of various antitumor agents aimed at gaining deeper understanding of the underlying mechanisms that may allow to develop new strategies for prevention and treatment of such formidable complications.
What is already known about this subject?
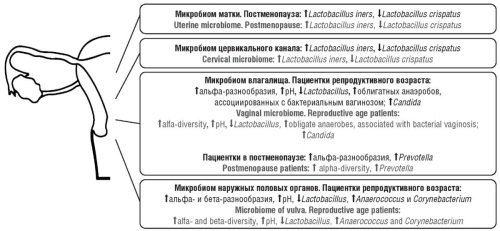
► Unlike the gut microbiome, which has been well studied in obese patients, the microbiome of the female reproductive tract is still under investigation.
► Normally, the lower female reproductive tract and endometrium is Lactobacillus-dominated microbiome.
► A decline in Lactobacillus abundance in all niches of the female genital tract is a risk factor for infertility, implantation failure, miscarriage, premature birth, endometriosis, and endometrial cancer.
What are the new findings?
► The article summarizes the data on the features of the microbiome of the external genitalia, vagina, cervical canal, uterus and ovaries. For the first time, a review of studies on the microbiome in all niches noted above in patients with overweight and obesity unrelated to and during pregnancy has been performed.
How might it impact on clinical practice in the foreseeable future?
► Overweight and obesity contribute to the pathogenesis of bacterial vaginosis by decreasing Lactobacillus abundance and elevating vaginal pH value.
► Weight loss is an independent factor allowing to restore normal Lactobacillus abundance.
High-throughput 16S rRNA sequencing has allowed us to identify novel microorganisms and their relationships in the female reproductive tract. However, in obese patients, the female reproductive tract microbiome, unlike the intestinal microbiome, has been understudied. Here, the literature review analyzes and describes microbiome features in the external genitalia, vagina, cervical canal, uterus, and ovaries in overweight and obese nonpregnant and pregnant females. The microbiome of the lower female reproductive tract in obese patients is characterized by increased bacterial diversity, pH, decreased Lactobacillus abundance, and increased abundance of obligate anaerobes and yeasts of the genus Candida. The endometrial microbiome in overweight and obese patients has been studied only in postmenopause and is characterized by higher Proteobacteria abundance. No data on the characteristics of the ovarian microbiome in obese patients are available. The mechanisms accounting for microbiome changes in obese patients are likely to due to the ability of adipose tissue-derived leptin and estrone to inhibit production of pituitary gonadotropic hormones resulting in blocked ovulation and lowered estradiol production in patients of reproductive age. Consequently, a decline in glycogen synthesis in the vaginal epithelium, decreased Lactobacillus abundance followed by elevated vaginal mucus pH value and number of obligate anaerobes, including those associated with bacterial vaginosis are observed. Weight loss can have a beneficial effect on the state of the vaginal microbiome, restoring normal Lactobacillus abundance.
What is already known about this subject?
► A significant number of chemicals found in the environment exert properties disrupting human endocrine system (endocrine disrupting chemicals, EDC).
► Many cases of idiopathic infertility are associated with EDC or direct and/or indirect effects of environmental factors.
► A negative correlation between EDC levels and reproductive function was found in both men and women.
What are the new findings?
► The combination of increased rainfall and high altitude during childbirth may have a positive effect on female fertility. Exposure to electromagnetic fields increases idiopathic infertility prevalence.
► Еxposure to heavy metals is associated with an increased risk of infertility during normal pregnancy and decreased number of eggs extraction during artificial insemination, whereas pesticide exposure reduces the likelihood of pregnancy and live birth.
► Exposure to bisphenol A (BPA) and fluorinated BPA (BPАF) has detrimental effects on viability of ovarian follicles, their function and maturation, lowering the number of eggs extracted, reducing embryos quality and chances for successful implantation.
How might it impact on clinical practice in the foreseeable future?
► Understanding presicely which environmental factors can negatively affect fertility and fetal development will help creating recommendations to alleviate their impact on a woman's body.
► Doctors will be able to take into account not only the genetic and physiological patients’characteristics, but also the environmental impact on their health. This may lead to development of new methods for treatment and rehabilitation aimed at restoring women's reproductive health.
► Understanding an impact of the environment on women's reproductive health can help creating a healthier and safer environment relying on development and implementation of environmental standards.
Introduction. The environment undoubtedly affects the physiological processes in human body, which may be both beneficial and harmful. From 2011 to 2021, the incidence of female infertility in Russia increased by 30 % reaching 789.1 cases per 100,000 women in 2021.
Aim: to assess an impact of environmental factors including endocrine disrupting chemicals (EDC) on women's reproductive health by assessing available publications.
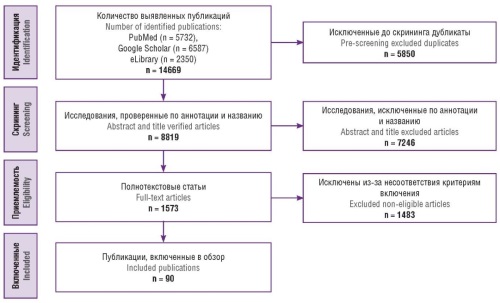
Materials and Methods. Available studies were searched through the scientific literature databases until April 2024 by revealing 5,732 articles in the PubMed/MEDLINE database, 6,587 in Google Scholar and 2,350 in eLibrary. The publications were selected in accordance with PRISMA recommendations. The current review included 90 publications.
Results. Fertility experimental and epidemiological studies showed that environmental factors such as climate, temperature, seasonality, radiation, air pollution, diet and energy balance, working environment, bad habits (e.g. smoking), EDC (plasticizers, heavy metals, parabens, pesticides, industrial chemicals and their by-products, medicines, perfluorochemicals, antibacterial agents) may be associated with impaired female reproductive function.
Conclusion. Environmental factors, including EDC, have a significant impact on women's reproductive health and can negatively affect fertility. The main findings of current research confirm a need to raise awareness of the risks associated with exposure to chemicals on women's body.
What is already known about this subject?
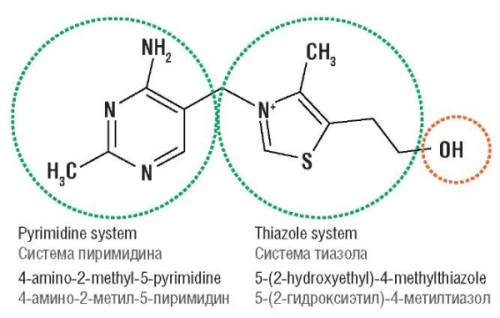
► Thiamine (vitamin B1) was previously used as uterotonics in 1940–1960’s. However, this practice seems to vanish in modern literature.
► Molecular structure of thiamine has been defined and its function is clear nowadays. Mainly as a coenzyme in energy metabolism.
► It’s often in Indonesia, especially in West Java used as uterotonics and cervical agent ripening in conjunction with misoprostol. Its usage still has no clear background/academic evidence.
What are the new findings?
► After literature review it was found in the 1940–1960s extensive research was perform with thiamine, and some research shows promising results.
► It’s hypothesize that effect of vitamin B1 on the uterine muscle, it’s promotes stimulation of uterine contractions by direct thiamine participation in development of nerve impulses.
► However recent founding shows cholinergic nerve supply of the human myometrium was found to be predominantly postganglionic and minimal. Thiamine also already known as coenzyme in energy metabolism which acetyl-CoA works. It could be concluded the most important function of thiamine largely contributes to the cellular energy metabolism not because it has effect on neuron impulses nor low uterine segment formation.
How might it impact on clinical practice in the foreseeable future?
► Educate midwifes, doctors, and residents that thiamin/vitamin B1 couldn’t be use as medication in cervical ripening.
► Administration of vitamin B1 could prove usable if the mother already had contraction and in hypovitaminosis condition. However this gave a little to no effects on normal pregnant and parturient patients.
► Reduce unneeded medication which reduces the cost of hospitalization for labour patient.
In Indonesia, thiamine (B1) has been use for cervical priming and enhancing uterine contraction in midwife and hospital setting as its off-label effect. However there are no clear evidence and research related to this issue. Thiamine itself was founded in 1990’s and has been used extensively as labour augmentation in 1940–1960’s. Main hypothesis previously due to B1 increased function of the uterine body and lower uterine segment obliteration during labour which also responsible for the reduction of pain. Thiamine also assumed to promote stimulation of uterine contractions by direct participation in nerve impulses that regulates and establish the rhythm of uterine contractions and also inhibits action of cholinesterase which reduce acetylcholine clearance. However recent research proves B1 mainly function in Krebs cycle specifically in decarboxylase of pyruvate to acetyl-CoA in form of thiamin diphosphate, synonymously known as thiamine pyrophosphate. Due to clear foundings of B1 function in cell energy metabolism, study of B1 in labour augmentation was not continue further. It’s also related to uterine contraction function in labour not relied on it’s paracervical parasympathetic ganglia which respond to acetylcholine but rely heavily on oxytocin and its receptor. As conclusion, the author stated B1 have no effect on labour progression however could prove beneficial if the mother has B1 deficiency as it’s could reduce energy output from cell which could affect myometrial contraction.
What is already known about this subject?
► The diagnosis of autism spectrum disorder (ASD) in children is based on clinical examination.
► Children are diagnosed around the age of 4.
What are the new findings?
► Using techniques such as magnetic resonance imaging and electroencephalography, it is possible to make early diagnoses as early as 6 months of age.
How might it impact on clinical practice in the foreseeable future?
► Early diagnosis of a child with an ASD could enable early therapeutic treatment.
► By taking advantage of the high degree of neuroplasticity in babies, the severity of the disease could be reduced.
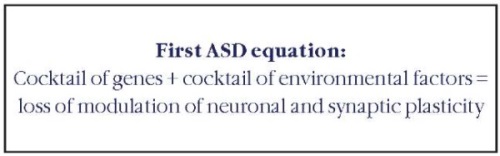
Autism spectrum disorder (ASD) is a neurodevelopmental condition that can be reliably diagnosed in children by age 18–24 months. Prospective longitudinal studies of infants aged 1 year and younger who are later diagnosed with autism are elucidating the early developmental course of autism and identifying ways of predicting autism before diagnosis is possible. Studies that use magnetic resonance imaging and electroencephalography, have identified differences in brain development in infants later diagnosed with autism compared with infants without autism. Retrospective studies of infants younger than 1 year who received a later diagnosis of autism have also showed an increased prevalence of health conditions, such as sleep disorders, gastrointestinal disorders, and vision problems. We propose two equations to describe this complex disorder: the first indicates the factors at the origin of the disease, the second synthesizes the different factors leading to a more or less severe disease. Although research findings offer insight on promising screening approaches for predicting autism in infants, individual-level predictions remain a future goal. Multiple scientific challenges and ethical questions remain to be addressed to translate research on early brain-based and behavioural predictors of autism into feasible and reliable screening tools for clinical practice.
CLINICAL CASES
What is already known about this subject?
► Uterine fibroid (UF) is a common disease of female reproductive sphere.
► Laparoscopic myomectomy is a mini-invasive route of surgical treatment.
What are the new findings?
► The introduction of morcellation into wide clinical practice allowed to expand the indications for laparoscopic myomectomy.
► Morcellation may have specific complication such as emergence of iatrogenic abdominal fibroids upon improper surgery technique.
► Morcellation of UF should be performed with a morcellation container.
How might it impact on clinical practice in the foreseeable future?
► This article helps to pay gynecologists’ attention to the need for performing myomectomy with laparoscopic access strictly in accordance with current guidelines.
► The main direction in UF treatment should rely on an individual approach based on assessing symptoms, node sizes, patient age and reproductive plans.
► The adequacy for choosing treatment strategy is determined by its efficiency and no-relapse outcome.
Introduction. Uterine fibroids are benign monoclonal hormone-sensitive tumors arising from smooth muscle cells of the cervix or body uterus. Myomectomy has become a treatment «golden standard» upon transition to the strategy of organ-preserving surgery. The introduction of morcellation into wide clinical practice allowed to expand the indications for laparoscopic myomectomy, which is usually much better tolerated by patients due to lower invasiveness, short period of rehabilitation and low blood loss. However, the use of morcellators along with the obvious advantages has also specific complications particularly emergence of iatrogenic parasitic fibroids of the abdominal cavity upon improper surgery technique.
Aim: analysis of a clinical case of multiple morcelloma.
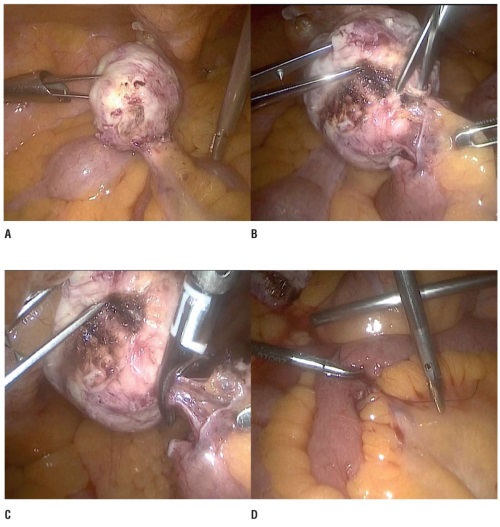
Case presentation. Female patient I., 57 years old, underwent laparoscopic myomectomy in 2003. In 2023 during a routine examination at the Central Clinical Hospital «RZD-Medicine» multiple asymptomatic iatrogenic fibroids of the abdominal cavity were revealed. The patient underwent planned surgical intervention to remove all abnormal masses.
Results. During the revision upon surgical intervention, a node of 1.5x1.5 cm was found on the parietal peritoneum along the left anterior wall, as well as a node of 1.5x1.5 cm on the parietal peritoneum along the right anterior wall. There was also observed a 2x3 cm node at the edge of the omentum. In the left and right side of peritoneum of the sacro-uterine ligament, there were found nodes of up to 1.0 cm in size. In the area of the small intestinal mesentery, a dense node of 4.5 cm was observed 70 cm away from the ileocecal valve. Due to small size, all the fibroids were extirpated and removed from the abdominal cavity without morcellation, complete hemostasis was performed. No complications were noted during postoperative period.
Conclusion. Iatrogenic fibroids are quite rare but nevertheless a potential complication of laparoscopic myomectomy. Gynecologists should pay special attention to follow proper technique upon surgical intervention. Morcellation and subsequent extraction of fibroids should be performed strictly with use of airtight container to avoid ingress of myomatous tissue into the abdominal cavity followed by emergence of iatrogenic fibroids.
What is already known about this subject?
► For a long time, continuity of therapy for patients with systemic juvenile idiopathic arthritis (sJIA) upon transition to the adult healthcare remained a serious problem, because most often it was accompanied by a change in diagnosis.
► Issues of reproduction in sJIA remain extremely poorly studied.
► The widespread introduction of anticytokine biological therapy into clinical practice is accompanied by new interdisciplinary tasks.
What are the new findings?
► The development of macrophage activation syndrome (MAS) during pregnancy is one of the most serious and potentially fatal complications.
► Treatment of MAS requires active and careful monitoring by entire interdisciplinary team.
How might it impact on clinical practice in the foreseeable future?
► It is necessary to focus on alertness of doctors from various specialties on the features of sJIA and MAS diagnostics and management while planning preconception preparation.
According to the current concept, juvenile arthritis with a systemic onset (systemic juvenile idiopathic arthritis, sJIA) and adultonset Still's disease (ASD) are considered as rare autoinflammatory diseases, with the underlying immunopathogenesis being based on the mechanisms bridging both of such diseases. Despite they develop in childhood and young age, the issues of reproduction occurring during these pathologies virtually unexplored. The article presents a clinical case of maternal death in a 22-year-old primiparous woman and analyzes the tactics of sJIA management, which was complicated by pregnancy-related macrophage activation syndrome.
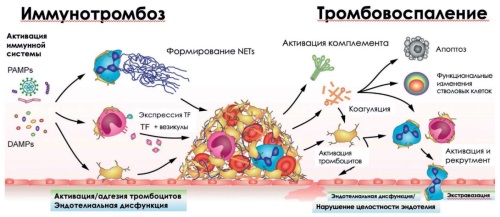
LECTURE
COVID-19 is one of the most dangerous diseases of the current decade that has significantly affected the overall morbidity, mortality, quality of health and life of global population. Among multiple early and late post-COVID complications observed in patients with a new coronavirus infection, perhaps the main place is held by thrombosis. The significant role of microthrombosis, disseminated intravascular coagulation, thrombotic angiopathies in COVID-19 pathogenesis is noted. The accumulated data from clinical studies and the presented expert opinions made it possible to establish the significance of the "immunothrombosis–NETosis–thromboinflammation" relationship in the pathological effects caused by SARS-CoV-2 virus, as well as to reveal the mechanisms underlying formation of thrombotic syndromes mediated by anticoagulant therapy and vaccination. The information obtained about hemostasis disorders allows to move deeper into understanding the long-term sequelae in COVID-19 convalescent patients.
FROM HISTORY
In December 19, 2024, there was the 90th anniversary of the birth of Ronald Andrew Asherson, a great scientist who prominently contributed to the development of medicine. His work in the field of clinical immunology, especially in the study of catastrophic antiphospholipid syndrome (CAPS), has become the basis for modern approaches to the diagnostics and treatment of this rare but dangerous disease. Asherson's discoveries notably widened the understanding of the mechanisms behind autoimmune disorders associated with phospholipids and improved the prognosis of CAPS patients. Asherson was not only the discoverer in studying CAPS, but also influenced a whole generation of scientists and clinicians. It is a great importance to preserve the memory about his life and scientific achievements for future generations of researchers and doctors who will continue to develop and use his ideas in practice.
With over 70 years of development, the Department of Obstetrics and Gynecology at Tianjin Medical University General Hospital has evolved into a comprehensive center for clinical care, research, and education, showcasing significant influence and technical strength in the field of obstetrics and gynecology. The department operates more than 200 beds, handles over 260,000 outpatient and emergency visits annually, and performs nearly 10,000 surgeries each year. As the final referral and rescue center for complex and critical cases in Tianjin, the department excels in sub-specialties such as perinatal medicine, gynecologic oncology, obstetric critical care, reproductive medicine, and gynecological endocrinology. It has made significant advances in precision diagnosis and personalized treatments, leading the development of the discipline in Northern China. In recent years, the department has demonstrated outstanding scientific innovation, undertaking numerous national and provincial-level projects, publishing high-impact papers, and contributing to multiple international and national guidelines. The department continues to advance both academic and clinical excellence, significantly contributing to the Healthy Tianjin Initiative and the broader Healthy China Action.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
ISSN 2500-3194 (Online)