Scroll to:
Debunking the myth: usage of thiamine in cervical preparation and labour augmentation
https://doi.org/10.17749/2313-7347/ob.gyn.rep.2024.568
Abstract
In Indonesia, thiamine (B1) has been use for cervical priming and enhancing uterine contraction in midwife and hospital setting as its off-label effect. However there are no clear evidence and research related to this issue. Thiamine itself was founded in 1990’s and has been used extensively as labour augmentation in 1940–1960’s. Main hypothesis previously due to B1 increased function of the uterine body and lower uterine segment obliteration during labour which also responsible for the reduction of pain. Thiamine also assumed to promote stimulation of uterine contractions by direct participation in nerve impulses that regulates and establish the rhythm of uterine contractions and also inhibits action of cholinesterase which reduce acetylcholine clearance. However recent research proves B1 mainly function in Krebs cycle specifically in decarboxylase of pyruvate to acetyl-CoA in form of thiamin diphosphate, synonymously known as thiamine pyrophosphate. Due to clear foundings of B1 function in cell energy metabolism, study of B1 in labour augmentation was not continue further. It’s also related to uterine contraction function in labour not relied on it’s paracervical parasympathetic ganglia which respond to acetylcholine but rely heavily on oxytocin and its receptor. As conclusion, the author stated B1 have no effect on labour progression however could prove beneficial if the mother has B1 deficiency as it’s could reduce energy output from cell which could affect myometrial contraction.
For citations:
Suryawan A.Z., Nisa A.Sh., Santoso D., Slamet S.A., Handono B. Debunking the myth: usage of thiamine in cervical preparation and labour augmentation. Obstetrics, Gynecology and Reproduction. 2024;18(6):874-881. https://doi.org/10.17749/2313-7347/ob.gyn.rep.2024.568
Introduction / Введение
Thiamine (vitamin B1) is important for human body due to its function as co-enzyme in cell powerhouse. Since its discovery by C. Eijkman (1890s) and establishment of B1 structure by R.R. Williams (1933), number of research had grown in many fields and one of them in obstetric field [1]. Usage of thiamine in labour induction quite popular in 1940’s until 1960’s, nowadays its usage shifted to pregnancy supplement [2–8]. However it’s quite common in Indonesia, B1 use for cervical priming and enhancing uterine contraction in midwife and hospital setting in conjunction with misoprostol and oxytocin. However, this practice has no clear evidence and clinical trials. In this article we wish to see why this practice has been considered and is it applicable in nowadays practice?
Thiamine and its function in cell energy pathway / Тиамин и его функция в энергетическом обмене клетки
Thiamin was first known by its deficiency and named ‘beriberi’ in English and ‘kakké’ in Japan and China [1]. Early hypothesis postulated beriberi was attributed to miasmas rising from wet soil and to an unknown infectious organism [1]. C. Eijkman in 1890s observed that chickens fed polished rice developed a polyneuritis, whereas chickens fed unpolished rice did not [1]. К. Takaki a naval surgeon in Japan also observed high occurrence of beriberi in warship crew in 1880s, after he loaded the navy with meat and dried milk the disease drastically reduce. К. Takaki then concluded that the disease experienced by the crew was closed related to foods [9][10]. Later on (1926), B.C.P. Jansen and his colleague W.F. Donath obtained anti-beriberi substance in crystal form obtained from the rice polishing process [11]. The research continued by R.R. Williams and J.K. Cline (1936) which define molecular structure of thiamin and later on could be manufactured in high volume [12].
Thiamin consists of a pyrimidine ring (2,5-dimethyl-6-aminopyrimidine) and a thiazolium ring (4-methyl-5-hydroxyethyl thiazole) linked by a methylene bridge. The primary sources of thiamin include meats, whole grains, liver, eggs, fish, legumes, and whole grains. Cooking processes involving heating, as well as the consumption of coffee and tea, can affect its availability [13][14]. Thiamin diphosphate (TDP) is a phosphorylated form of thiamin that serves as a crucial cofactor in various enzymatic reactions. Its three primary functions include activating the decarboxylation of pyruvate into the pyruvate dehydrogenase complex, decarboxylation in alpha-ketoglutarate dehydrogenase, an important component of the citric acid cycle, and in the macromolecular aggregation that decarboxylates keto acids [15][16].
Free thiamine is initially phosphorylated to form biochemically active TDP, synonymously known as thiamine pyrophosphate (TPP). TPP possesses a crucial structural element in the form of a thiazolium ring, a five-membered heterocyclic ring containing sulfur and positively charged nitrogen atoms (Fig. 1) [17]. TPP acts as a coenzyme for thiamine for transketolase (TK) in the pentose phosphate pathway, for pyruvate dehydrogenase (PDH) in the glycolysis, and for alpha-ketoglutarate dehydrogenase (AKD) in the Krebs cycle [17][18]. Each of these enzymes can only fulfill its function with thiamine help (Fig. 2). Then, acetyl-CoA will play a role in providing the acetyl molecule needed to initiate the Krebs cycle, which is an essential part of cellular metabolism and generates a lot of energy in the form of adenosine triphosphate (ATP) [18].
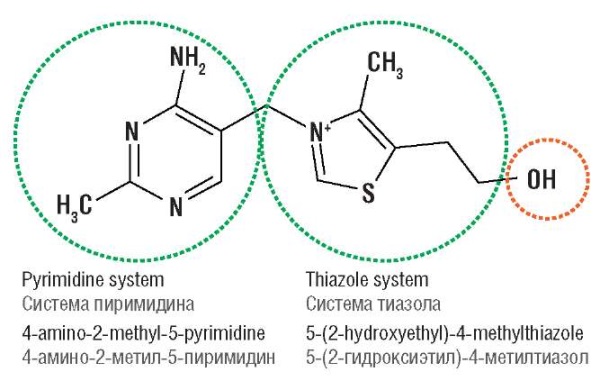
Figure 1. Thiamine molecular structure [17].
Рисунок 1. Молекулярная структура тиамина [17].
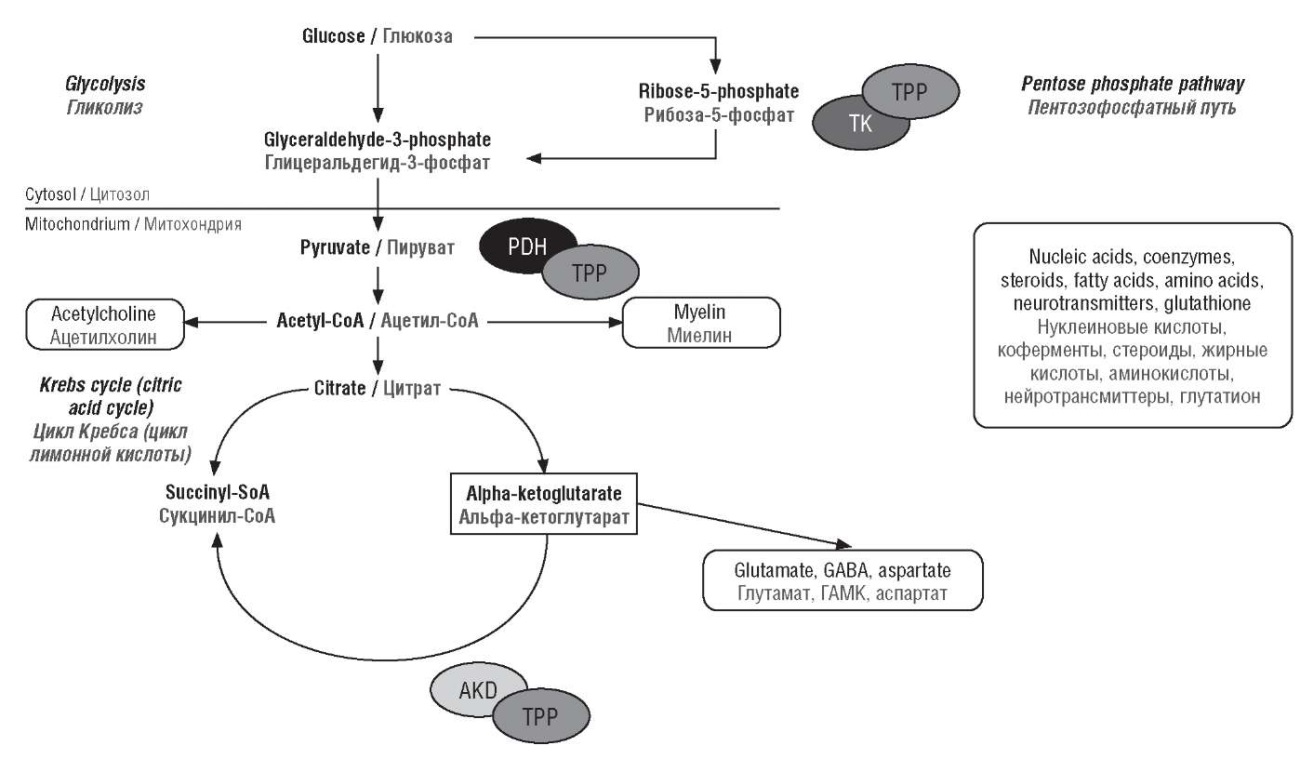
Figure 2. Biochemical mechanism of vitamin B1 (thiamine) action [18].
Note: TPP – thiamine pyrophosphate; TK – transketolase; PDH – pyruvate dehydrogenase; AKD – alpha-ketoglutarate dehydrogenase; CoA – coenzyme A; GABA – gamma-aminobutyric acid.
Рисунок 2. Биохимический механизм действия витамина B1 (тиамина) [18].
Примечание: TPP – тиаминпирофосфат; TK – транскетолаза; PDH – пируватдегидрогеназа; AKD – альфа-кетоглутаратдегидрогеназа; CoA – коэнзим А; GABA – гамма-аминомасляная кислота.
Due B1 large involvement in energy pathways, the deficiency of thiamine limits the supply of enzymes to the Krebs cycle leading to decreased ATP, oxidative damage, and cell death [18][19]. Decreased TK activity impairs synthesis of nucleic acids and glutathione, mainly affect the central nervous system (CNS) which is highly dependent on ATP generated by oxidative decarboxylation. Through triggering N-methyl-D-aspartate (NMDA) toxicity and increasing apoptotic cell death Wernicke's encephalopathy and Korsakoff's psychosis occurs in B1 deficiency [18][20].
Thiamine usage in labour induction and augmentation / Использование тиамина для индукции и стимуляции родов
From PubMed search engine we found that this practice is popular in 1940’s–1960’s [2–8]. The earliest article we could found is from S.S. Zilberman (1949) which stated thiamine could increase uterine activity in labour. The author explained from his experiment with animal subject pregnant uterus reacts to thiamine with increase of contractility and tone as shown in Figure 3. Не concluded thiamine stimulates uterine contractility with expressed as increase of uterine tone and frequency of contraction [2].
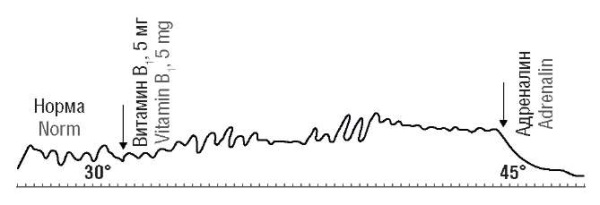
Figure 3. Uterine contraction of pregnant white mouse (40 g) after admission of 5 mg thiamine [2].
Рисунок 3. Сокращение матки беременной белой мыши (40 г) после введения 5 мг тиамина [2].
S. Lorand et al. (1952) perform large trial of thiamine with dosage of 50 mg and with/without 3 U of glanduitrin at parturient patient with 2 cm dilation. In 50 % of cases, the amplitude of contractions was increased followed by birth accelerated in one of third of cases. The authors also found intensity of pain was reduced in 38 % of cases and in 55 % of cases dilation progression was not accompanied by an increase in pain. They concluded acceleration of childbirth is due to increased function of the uterine body and lower uterine segment obliteration during labour which also responsible for the reduction of pain [6]. High variability in this study needed to be questioned as such the contraction mainly due to it already starts to adequate due time or the effect of oxytocin given in conjunction with B1 (Fig. 4).
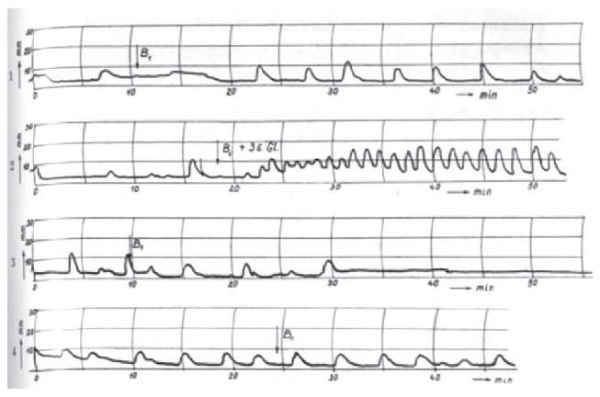
Figure 4. Uterine tocography of pregnant white mouse (40 g) after admission of 5 mg thiamine [6].
Note: 1 – shows after injection of thiamine contraction became adequate; 2 – injection of thiamine and glanduitrin followed by adequate and strong contraction; 3, 4 – of thiamine injection does not affect contraction with different patent.
Рисунок 4. Токография матки беременной белой мыши (40 г) после введения 5 мг тиамина [6].
Примечание: 1 – показано, что после инъекции тиамина сокращение стало адекватным; 2 – инъекция тиамина и гландуитрина сопровождается адекватным и сильным сокращением; 3, 4 – инъекция тиамина не влияет на сокращение с различной степенью выраженности.
In early 1900’s a lot of researchers observed thiamine have a favorable effect in cases of uterine inertia. S. Timonen and K.A. Schroderus (1953) hypothesized that aneurin inhibits action of cholinesterase in which way delayed acetylcholine clearance [21]. This mechanism similar with prostigmin which was use in the past for labour induction or neostigmin in nowdays practice to reverse muscle relaxation during general anaesthesia for caesarean section [22][23].
H.J. Prill (1954) divided 171 patients as subject into 2 individual groups, first one 100 primiparous women over 18 years of age as group A and 71 primiparous and multiparous women with primary or secondary hypotonic labor weakness as group B, which both group received 900 mg of vitamin B1 (Benerva, Betabion or Betaxin) intra-muscular found that vitamin B shortens duration of labour from 11.08 hours to 9.5 hours in 52 subjects [4]. Based on previous research, K.F. Zalevskaya (1961) performs an isolated study for labour induction using thiamine. She concluded that the most effective dose is 240 mg administered by two injections of 6 mL of 2 % thiamine solution with one hour interval. The author also hypothesize this positive outcome due the effect of vitamin B1 on the uterine muscle, it’s promotes stimulation of uterine contractions by direct thiamine participation in development of nerve impulses that regulate and establish the rhythm of uterine contractions [24].
However in contrary, a lot of researchers contradict thiamine role in shortening of labour. Even H.J. Prill (1954) concluded general use of vitamin B1 does not produced any statistically significant shortening of labour [4]. E. Szirmai (1961) also conducted the induction of labour with 50 mg of thiamine in 1962 and found in 29 births only 2 patients had their contraction increased and the rest of the cases it did not change [5].
Thiamine, oxytocin and neuroendocrine pathway of uterine contraction / Тиамин, окситоцин и нейроэндокринный путь сокращения матки
Thiamine has long-known effect on nervous system. Deficiency of thiamine leads to many dire situations such as thiamine-deficient disease we called beriberi. Early manifestation shows mainly in disturbance of peripheral nerve disease and in later stage manifest as encephalopathy (Wernicke’s encephalopathy) [18][25]. Previously it was hypothesized that thiamine plays same roles as acetylcholine in excitatory pathway of nerve and later it was hypothesized thiamine inhibits cholinesterase [20][26].
Myometrial contractions are a hallmark of parturition, both at term and preterm [27]. Contraction of each myocyte causes by intracellular calcium (Ca2+) accumulation. This induce myosin phosphorylation which increased actin-myosin crosslinks and contraction [27][28]. From biochemical perspective it’s induce with increasing levels of matrix metalloproteinase (MMP), interleukin-6 (IL-6), interleukin-8 (IL-8) and cyclooxygenase-2 (COX-2) in concurrence of progesterone withdrawal and its associated receptors [27][29]. Progesterone withdrawal increases myocytes estrogen responsiveness and it’s receptors which leads to increase sensitivity to oxytocin [27][29].
Oxytocin is a neuropeptide that produces by neurosecretory cells within the paraventricular nucleus (PVN) and the supraoptic nucleus (SON) in the hypothalamus and secreted through neurohypophysis [30]. Oxytocin then released to blood and affect targeted organ, and in this case uterine contraction [29][30]. The brain and uterus connected with what so called Ferguson Reflex which is afferent neural pathway that involves mechanical stretching of the cervix enhances uterine activity [29][30]. Role of autonomic innervation in uterine contraction has been recognize in older research and publication but had not gain attention in newer research [32]. Y. Sato et al. (1996) showed stimulation of the efferent pelvic nerve with supramaximal intensity induced increase in uterine blood flow accompanied by uterine contraction. However, efferent hypogastric nerve stimulation caused decrease of uterine blood flow accompanied by uterine contraction. These founding leads to conclusion that terine contraction is produced by activation of both parasympathetic and sympathetic nerves via muscarinic cholinergic receptors [33]. This also supported by R.E. Papka et al. (1999) founding that paracervical parasympathetic ganglia contains a lot of muscarinic receptors which will respond acetylcholine [34].
Whether the activity of the autonomic nervous system plays a role in human labor and delivery is not known due degenerative changes during pregnancy, as demonstrated both in animal studies and in women [35]. H. Nakanishi and C. Wood (1971) found intrinsic cholinergic nerve supply of the human myometrium was found to be predominantly postganglionic and minimal. They also found markedly decreased sensitivity of pregnant muscle to acetylcholine when compared to non-pregnant muscle [36]. However, such degenerative changes do not occur in uterus cervix, where the innervation remains intact. Therefore, nervous activity may still play an important role in labor alongside oxytocin [32][35]. It could be concluded the most important function of thiamine largely contributes to the cellular energy metabolism because thiamine is an essential cofactor in the carbohydrates cycle [18].
Misoprostol and thiamine / Мизопростол и тиамин
Misoprostol is a synthetic prostaglandin E1 (PGE1) analog which binds strongly to prostaglandin E2 (PGE2) receptors subtypes EP3 and also EP2 [37][38]. Binding with prostaglandin E2 receptors increase phospolipase C, which increase influx of Ca2+ intracellular that will lead on uterine contraction and also induce inflammation in the cervix, which recruits macrophages that later induce cervix ripening [38].
Cervical ripening induced by PGE1 and PGE2 is associated with an increase in inflammatory mediators in the cervix, and remodeling of the cervical extracellular matrix through a decrease in collagen cross links and cervical glycosaminoglycans [38]. It’s quite contrary with thiamine which is anti-inflammatory. Thiamine itself has been proven to reduced C-reactive protein (CRP) and expression of tumor necrosis factor-alpha (TNF-α) in gestational diabetes patients [39]. Thiamine also has better antioxidant effect compared to ascorbic acid with reducing MMP-9 level in sepsis patients [40]. These facts already enough to debunk the myth of thiamine usage in labour induction or augmentation. Its effect on cell cycle indeed provides constant ATP within uterine muscle but not to the extent of enhancing contraction and help cervical ripening.
Conclusion / Заключение
Thiamine don’t have sufficient prove for usage in labour induction and augmentation. It’s has anti-inflammatory effects and contradict the misoprostol function which promotes the level of prostaglandin and others inflammatory cytokines in the cervix. Previously B1 assumed to perform in neural excitation and help achieve routine contraction. However previous research at 1940–1960’s couldn’t provide clear mechanism and procedure on how thiamine works.
References
1. Carpenter K.J. The discovery of thiamin. Ann Nutr Metab. 2012;61(3):219-23. https://doi.org/10.1159/000343109.
2. Zilberman S.S. Effect of vitamin B1 on uterine contractibility. [Vliyanie vitamina V1 na sokratitel'nuyu sposobnost' matki]. Akusher-ginekolog (Moskva). 1949;34(1):27-30. (In Russ.).
3. Lorand S., Szirmai E., Csizmadia Z. Effect of vitamin B1 on labor pains and activity. Orv Hetil. 1951;92(25):788-92.
4. Prill H.J. The effects of vitamin B1 on uterine contraction and length of labor. Zentralbl Gynakol. 1954;76(14):548-52.
5. Szirmai E. Thiamine (vitamin B 1) and its effects on the uterine musculature and on the pain during delivery (preliminary report). Zentralbl Gynakol. 1961;83:554-5. [In German].
6. Lorand S., Szirmai E., Csizmadia Z. Tokographic analysis of the effect of vitamin B1 on the effectivity of labor pains and on labor pain sensitivity. Gynaecologia. 1952;133(3):155-63.
7. Korolowa S. Vitamin B1 as a drug inducing labor and increasing labor pains. Przegl Lek. 1952;8(7):199-201.
8. Triantafillopoulo B. Rapid childbirth: biological effect of thiamine (vitamin B1) on the muscular fiber of the gravid uterus. Gynecol Obstet. 1958;57(3):313-26. [In French].
9. Takaki K. On the cause and prevention of kak'ke. Trans Sei-I-Kwai. 1885;39(Suppl 4):29-37. [In Japanese].
10. Inouye K. Etiology and pathology of beriberi. In: Review of Japanese literature on beriberi and thiamine. Eds. N. Shimazono, E. Katsura. Igaku Shoin Ltd, 1965. 1-28.
11. Jansen B.C.P., Donath W.F. On the isolation of the anti-beri-beri vitamin. Proc Konink Akad van Wetensch Amsterdam. 1926;107:1390-400.
12. Williams R.R., Cline J.K. Synthesis of vitamin B1. J Am Chem Soc. 1936;58:1504-5.
13. Flodin N.W. Pharmacology of micronutrients. In: Current topics in nutrition and disease.USA: A.R. Liss, 1988. 340 p.
14. Lonsdale D. A review of the biochemistry, metabolism and clinical benefits of thiamin (e) and its derivatives. Evid Based Complement Alternat Med. 2006;3(1):49-59. https://doi.org/10.1093/ecam/nek009.
15. Cole L.A., Kramer P.R. Human physiology, biochemistry and basic medicine. Academic Press: Elsevier Inc., 2015. 248 р.
16. Mrowicka M., Mrowicki J., Dragan G., Majsterek I. The importance of thiamine (vitamin B1) in humans. Biosci Rep. 2023;43(10):BSR20230374. https://doi.org/10.1042/BSR20230374.
17. McMurry E.J. Organic Chemistry. Houston, Texas: OpenStax, 2023. 1247 р.
18. Calderon-Ospina C.A., Nava-Mesa M.O. B Vitamins in the nervous system: Current knowledge of the biochemical modes of action and synergies of thiamine, pyridoxine, and cobalamin. CNS Neurosci Ther. 2020;26(1):5- 13. https://doi.org/10.1111/cns.13207.
19. WHO. Thiamine Deficiency and its Prevention and Control in Major Emergencies. Geneva, Switzerland: World Health Organization, 1999. 52 р. Available at: https://www.who.int/publications/i/item/WHO-NHD-99.13. [Accessed: 15.09.2024].
20. Sriram K., Manzanares W., Joseph K. Thiamine in nutrition therapy. Nutr Clin Pract. 2012;27(1):41-50. https://doi.org/10.1177/0884533611426149.
21. Timonen S., Schroderus K.A. The effect of aneurin on uterine contractions. Scand J Clin Lab Invest. 1953;5(3):207-11. https://doi.org/10.3109/00365515309094187.
22. Michalak W. Effect of prostigmine on uterine contractions during labor. Annales Academiae Medicae Bialostocensis.1967;13:109-37.
23. Radkowski P., Jacewicz M., Podhorodecka K. The use of muscle relaxants in pregnancy and puerperium period. Int J Gen Med. 2023;16:859-64. https://doi.org/10.2147/IJGM.S393885.
24. Zalevskaya K.F. On the use of vitamin B1 to enhance labor. [O primenenii vitamina V1 dlya usileniya rodovoj deyatel'nosti]. Kazanskij medicinskij zhurnal. 1961;42(1):44-6. (In Russ.).
25. Hassan M., Rahman H., Yasmeen B.H. et al. Thiamine deficiency - Beriberi - A forgotten disease. Northern International Medical College Journal. 2018;10:351-4.
26. Chiancone F.M. Vitamin B1 and autonomic drugs: a reprint. Acta Vitaminol Enzymol. 1977;31(6):195-206. [In Italian].
27. Resnik R., Lockwood C.J., Moore T.R. et al. Creasy and Resnik's maternal-fetal medicine: principles and practice. Philadephia, PA: Elsevier, 2019. 1388 р. Available at: https://nls.ldls.org.uk/welcome.html?ark:/81055/vdc_100064285917.0x000001. [Accessed: 15.09.2024].
28. Young R.C. Myocytes, myometrium, and uterine contractions. Ann N Y Acad Sci. 2007;1101:72-84. https://doi.org/10.1196/annals.1389.038.
29. Cunningham F.G., Leveno K.J., Dashe J.S. et al. Physiology of Labor. Williams Obstetrics, 26e. New York, NY: McGraw Hill, 2022. 1344 p.
30. Walter M.H., Abele H., Plappert C.F. The role of oxytocin and the effect of stress during childbirth: neurobiological basics and implications for mother and child. Front Endocrinol. 2021;12:742236. https://doi.org/10.3389/fendo.2021.742236.
31. Brunton P.J., Russell J.A.. Chapter 44 - Maternal Brain Adaptations in Pregnancy. In: Knobil and Neill's Physiology of Reproduction (Fourth Edition). Eds. T.M. Plant, A.J. Zeleznik. San Diego: Academic Press, 2015. 1957-2026.
32. Uvnas-Moberg K. The physiology and pharmacology of oxytocin in labor and in the peripartum period. Am J Obstet Gynecol. 2024;230(3S):S740- S758. https://doi.org/10.1016/j.ajog.2023.04.011.
33. Sato Y., Hotta H., Nakayama H., Suzuki H. Sympathetic and parasympathetic regulation of the uterine blood flow and contraction in the rat. J Auton Nerv Syst. 1996;59(3):151-8. https://doi.org/10.1016/0165-1838(96)00019-7.
34. Papka R.E., Traurig H.H., Schemann M. et al. Cholinergic neurons of the pelvic autonomic ganglia and uterus of the female rat: distribution of axons and presence of muscarinic receptors. Cell Tissue Res. 1999;296(2):293-305. https://doi.org/10.1007/s004410051290.
35. Owman C. Pregnancy induces degenerative and regenerative changes in the autonomic innervation of the female reproductive tract. Ciba Found Symp. 1981;83:252-79. https://doi.org/10.1002/9780470720653.ch13.
36. Nakanishi H., Wood C. Cholinergic mechanisms in the human uterus. J Obstet Gynaecol Br Commonw. 1971;78(8):716-23. https://doi.org/10.1111/j.1471-0528.1971.tb01635.x.
37. Allen R., O'Brien B.M. Uses of misoprostol in obstetrics and gynecology. Rev Obstet Gynecol. 2009;2(3):159-68.
38. Chiossi G., Costantine M.M., Bytautiene E. et al. The effects of prostaglandin E1 and prostaglandin E2 on in vitro myometrial contractility and uterine structure. Am J Perinatol. 2012;29(8):615-22. https://doi.org/10.1055/s-0032-1311986.
39. Amirani E., Aghadavod E., Shafabakhsh R. et al. Anti-inflammatory and antioxidative effects of thiamin supplements in patients with gestational diabetes mellitus. J Matern Fetal Neonatal Med. 2022;35(11):2085-90. https://doi.org/10.1080/14767058.2020.1779212.
40. Lubis B., Lelo A., Amelia P., Prima A. The effect of thiamine, ascorbic acid, and the combination of them on the levels of matrix metalloproteinase-9 (MMP-9) and tissue inhibitor of matrix metalloproteinase-1 (TIMP-1) in sepsis patients. Infect Drug Resist. 2022;15:5741-51. https://doi.org/10.2147/IDR.S378523.
About the Authors
A. Z. SuryawanIndonesia
Alfonsus Zeus Suryawan, MD.
Bandung, West Java
A. Sh. Nisa
Indonesia
Aisyah Shofiatun Nisa, MD
Bandung, West Java
D.P.J. Santoso
Indonesia
Dhanny Primantara Johari Santoso, MD.
Garut, West Java
S. A. Slamet
United States
Syamsudin Ahmad Slamet
Tulane Avenue, New Orleans, LA 70112
B. Handono
Indonesia
Budi Handono, MD, Dr Sci Med, Prof.
Bandung, West Java
What is already known about this subject?
► Thiamine (vitamin B1) was previously used as uterotonics in 1940–1960’s. However, this practice seems to vanish in modern literature.
► Molecular structure of thiamine has been defined and its function is clear nowadays. Mainly as a coenzyme in energy metabolism.
► It’s often in Indonesia, especially in West Java used as uterotonics and cervical agent ripening in conjunction with misoprostol. Its usage still has no clear background/academic evidence.
What are the new findings?
► After literature review it was found in the 1940–1960s extensive research was perform with thiamine, and some research shows promising results.
► It’s hypothesize that effect of vitamin B1 on the uterine muscle, it’s promotes stimulation of uterine contractions by direct thiamine participation in development of nerve impulses.
► However recent founding shows cholinergic nerve supply of the human myometrium was found to be predominantly postganglionic and minimal. Thiamine also already known as coenzyme in energy metabolism which acetyl-CoA works. It could be concluded the most important function of thiamine largely contributes to the cellular energy metabolism not because it has effect on neuron impulses nor low uterine segment formation.
How might it impact on clinical practice in the foreseeable future?
► Educate midwifes, doctors, and residents that thiamin/vitamin B1 couldn’t be use as medication in cervical ripening.
► Administration of vitamin B1 could prove usable if the mother already had contraction and in hypovitaminosis condition. However this gave a little to no effects on normal pregnant and parturient patients.
► Reduce unneeded medication which reduces the cost of hospitalization for labour patient.
Review
For citations:
Suryawan A.Z., Nisa A.Sh., Santoso D., Slamet S.A., Handono B. Debunking the myth: usage of thiamine in cervical preparation and labour augmentation. Obstetrics, Gynecology and Reproduction. 2024;18(6):874-881. https://doi.org/10.17749/2313-7347/ob.gyn.rep.2024.568

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.











































