Scroll to:
New perspectives on autism: two equations to describe a complex disorder and envisage new treatments
https://doi.org/10.17749/2313-7347/ob.gyn.rep.2024.526
Abstract
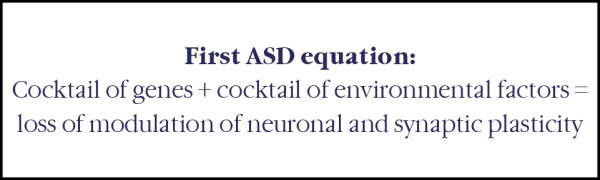
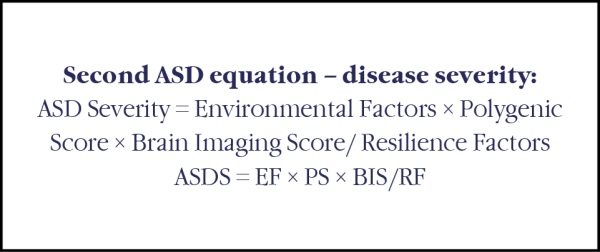
Autism spectrum disorder (ASD) is a neurodevelopmental condition that can be reliably diagnosed in children by age 18–24 months. Prospective longitudinal studies of infants aged 1 year and younger who are later diagnosed with autism are elucidating the early developmental course of autism and identifying ways of predicting autism before diagnosis is possible. Studies that use magnetic resonance imaging and electroencephalography, have identified differences in brain development in infants later diagnosed with autism compared with infants without autism. Retrospective studies of infants younger than 1 year who received a later diagnosis of autism have also showed an increased prevalence of health conditions, such as sleep disorders, gastrointestinal disorders, and vision problems. We propose two equations to describe this complex disorder: the first indicates the factors at the origin of the disease, the second synthesizes the different factors leading to a more or less severe disease. Although research findings offer insight on promising screening approaches for predicting autism in infants, individual-level predictions remain a future goal. Multiple scientific challenges and ethical questions remain to be addressed to translate research on early brain-based and behavioural predictors of autism into feasible and reliable screening tools for clinical practice.
For citations:
Suare B., Jeune M. New perspectives on autism: two equations to describe a complex disorder and envisage new treatments. Obstetrics, Gynecology and Reproduction. 2024;18(6):882-890. https://doi.org/10.17749/2313-7347/ob.gyn.rep.2024.526
Introduction / Введение
Once considered a rare and incurable disease, autism spectrum disorders (ASDs) are now the focus of an intense research effort to better understand, diagnose and treat them. Worldwide, between 1 and 2 % of the population is directly affected by ASDs, which are part of a broader group of neurodevelopmental disorders (NDDs) affecting one in six people. While research has made considerable progress over the last two decades, transforming the way autism is viewed and represented, we thought it would be interesting to take stock of recent scientific advances concerning ASDs, and early diagnosis methods enabling early treatment to be proposed [1].
Redefining autism / Переосмысление аутизма
ASDs are part of NDDs, which are particularities of brain functioning that also include "dysdisorders" (dyspraxia, dyslexia, dysphasia), attention deficit disorders with or without hyperactivity (ADHD), intellectual deficit disorders and certain epilepsies. Autism is characterized by communication and interaction disorders, restricted interests, sensory atypia and stereotypies (repetitive and seemingly aimless motor behaviors that the patient seems compelled to perform). There can be a wide variety of expressions, depending on whether or not autism is associated with an intellectual deficit or camouflage behaviours in a person with a high level of performance and learning. Diagnosis is clinical, based on symptoms that usually appear in the 2nd or 3rd year of life. It is a chronic disease, which can be associated with functional deficits, mental disorders and poor quality of life. Autism is four times more common in boys than in girls. The etiology is complex and heterogeneous. Genetic and environmental factors combine and converge to modify brain development before birth and during the first year of life. There is no routinely usable biomarker, and no effective pharmacological treatment.
Twin analyses and family studies show that genetics make a very strong contribution to autism. The 1st genes were identified in 2003, when monogenic forms were revealed. A single mutated gene, even a single copy of the gene, can cause autism, intellectual disability or a total absence of spoken language. Sometimes, a major gene is involved in less severe forms, in people who speak very well and have normal or even high IQ (intelligence quotient). The influence of genetic mutations is highly variable. Some genetic variations lead inexorably to a diagnosis of autism, while for other mutations, people will be diagnosed less often. Either because they are not autistic, or because they have not had access to diagnosis, or because the signs are less tangible. Take the image of an opera orchestra: if the singer stops singing, you can hear it right away. On the other hand, if the 5th violin stops playing, it's much less perceptible. But if several violins stop playing at the same time, there's a real difference. Not all genetic variations have the same consequences. Some will have a strong impact, while others, more common in the population, will play a more subtle role. It is the accumulation of the latter that will increase the probability of being diagnosed with autism. Monogenic forms of autism are mostly those with intellectual deficits. When a complete genome analysis of the individual and his or her parents is carried out, a genetic originis found in 30 to 40 % of cases of autism with intellectual disability. It is estimated that here are around 1,700 genes involved in neurodevelopment, and just over 200 which, when mutated, give a high probability of autism. On the other hand, polygenic forms correspond to more frequent variations in the population and are responsible for less severe ASD, without intellectual disability. To use the metaphor of an orchestra, these variants are like violinists, each playing a small score. Together, they produce a musical piece. These mutations give rise to particularities in the brains of autistic people [2–3].
Mislabeled neuro-visual disorders / Неправильно диагностированные нейровизуальные расстройства
Neuro-visual disorders, such as an inability to follow the gaze, can give rise to an autistic clinical picture. These neuro-visual disorders can interfere with the child's ability to interact with the outside world, and parents may interpret this as an autistic disorder. This autistic-like clinical pictureis the direct consequence of neuro-visual disorders. But not all children with neuro-visual disorders are autistic. There are educational environmental factors that protect against interaction disorders. People with autism often have visual features that resemble the visual features of those with neuro-visual disorders without autism. Ultimately, there is no visual difference between the two. It has long been taken for granted that autistic people see and hear normally, but primary etiological factors may have been overlooked, especially as these children are difficult to examine. We are often only interested in the visual or auditory acuity aspects, and not in the central cerebral aspects. Basic disorders may hinder social interaction and predispose to interaction disorders. Any sensory disorder predisposes to interaction disorders. We know, for example, that there are 40 times more cases of autism in visually impaired children than in the general population [4].
Are autism spectrum disorders connecttopathies and synaptopathies? / Являются ли расстройства аутистического спектра коннектопатиями и синаптопатиями?
Neurons communicate with each other via white matter fibers and synapses. There are around 10,000 synapses per neuron. Neurons make up the gray matter. White matter can be divided into 2 categories: deep white matter (or long-distance connectome) and superficial white matter (or short-distance connectome). The latter connects the cerebral convolutions to each other and contains a large number of neurons. This complex area, implicated in autism, is known as the 3rd brain substance. The biological role of the genes involved in ASD concerns the functioning of synapses, the connections between neurons. This is now better understood. In some cases, there are slightly fewer synapses, in others more synapses, i.e. a little more or a little less connectivity between neurons. These particularities could explain various ASDs symptoms, such as difficulty adapting to changes in routine and environment, as well as hypo- or hypersensoriality, notably to light, smells and tastes. Digestive disorders are also very common. The human enteric nervous system (ENS) contains 400 million neurons. According to recent research, dysfunction of the short-distance connectome explains the social cognition deficit in autistic patients [5–7].
Non-genetic causes of autism / Негенетические причины аутизма
The bulk of autistic subjects probably have no genetic abnormality, but a neurodevelopmental impairment linked to deleterious neurological events around birth. The neurological factors that predispose to autism are the same as those that predispose to other NDDs. Prematurity, certain medications such as Depakine during pregnancy, antibiotics, a lack of certain nutrients (vitamin B9, linoleic acid, omega-3, iron, zinc, iodine), pollutants (endocrine disruptors, emulsifiers), viruses and neuro-inflammation are all events that can be responsible for ASDs, but also for NDDs. This often results in a tangle of different manifestations, with overlapping diagnoses. For example, 50 % of people with autism have ADHD, and 30 % of people with ADHD also have autism.
Prenatal and postnatal exposure to pollutants such as endocrine disruptors, certain emulsifiers and PFASs (perfluoroalkylated and polyfluoroalkylated substances) play a key role in the onset of ASD. Exposure to a single productis not enough. Research by an international team has shown that a cocktail of at least 4 or 5 chemicals is necessary for the disorder to appear. These chemicals are omnipresent in our environment: cosmetics, kitchen utensils, plastics, furniture, food, drinking water, etc. We are all contaminated by these products to varying degrees. It is this kind of cocktail of chemicals that is responsible for the extinction of bees in areas of the world where pesticides are used [8–10].
A recent study has shown that ASDs children undergo profound changes in their intestinal microbiota at a very early age. These disturbances in the microbiota, known as dysbios is, show an imbalance in the intestinal flora, with an excess of Citrobacter-type bacteria and a deficiency of Coprococcus and Akkermansia muciniphila bacteria, which may be at the root of neuroinflammation. This dysbiosisis often linked to the early use of antibiotics in pregnant women and their babies. Coprococcus and Akkermansia play a vital role in the metabolism of vitamin B and the synthesis of neurotransmitter precursors, molecules essential to the proper functioning of synapses and neurons. Neurotransmitters play a vital role in orchestrating the electrical and chemical signals of neurons in the brain. It is estimated that 90 % of neurotransmitters are produced by intestinal bacteria. This imbalance disrupts the baby's immunity and also plays a role in the onset of type I diabetes and juvenile rheumatism. The discovery of this dysbiosis may justify fecal transplants in ASDs children, who often have severe digestive problems, with encouraging results in terms of intestinal symptoms and social cognition. It also justifies supplementing the diet of expectant mothers with vitamin B9, iron, iodine, zinc and omega-3 fatty acids [11][12].
So it's vital to consider ASD as a disease that affects the whole body, not just the brain.
Improving diagnosis and support for people with autism / Повышение качества диагностики и поддержки людей с аутизмом
While autism has long been caricatured as a childhood condition, it now spans the whole of life, and it is vital that all healthcare professionals – doctors, midwives, psychologists, speech therapists and occupational therapists – are better trained. ASDs are not just brain disorders. They also affect the whole body. Research is also exploring ways to better include people with autism, particularly in the urban environment. There is a new research approach in architectural neurology to creates paces adapted to the particularities of autistic people: housing estates with, in particular, softer perspectives, alcoves, modularity, more subdued lighting and easier circulation. The next step will be to promote the concept of neurodiversity, which enables us to celebrate the diversity of ways of thinking, and to demedicalize what used to be thought of as pathological in order to enable greater inclusion.
Three key brain regions for social cognition to better understand autism / Три ключевые области мозга, отвечающие за социальное познание и лучшее понимание аутизма
The cerebellum is a kind of mini-brain housed at the back of the brain. It contains 3 times as many neurons as the cerebral hemispheres. It has extremely sophisticated wiring, giving it enormous computational capacity. The cerebellumis an organ that coordinates movement and balance. It is also involved in social behavior and a large number of higher cognitive functions, notably emotional memory. It regulates social interaction, aggression, working memory, learning and emotions. There are specific neurodynamics in social interactions between the cerebral cortex and the cerebellum. These neuro-dynamics are particular to autistic patients. There are currently research protocols for trans-cranial magnetic stimulation of the cerebellum in autistic patients [13].
The second region implicated in autistic disordersis the ventral striatum. This particular brain region ensures motor control, is part of the reward circuit, plays a role in social interactions and in the selection of sensory information. There is a particular balance between the neuronal populations located in the ventral striatum that enables social behaviors to be controlled.
The third key brain regionis the parietal lobe. This lobe is an important integrative zone, generating self-awareness, managing social relationships and proprioception (the body's position in space). The parietal lobe is particularly voluminous in Homo sapiens. It is both the eye and the conductor of the other brain regions. The development of the parietal lobe, enabling coordination of hand and vision, enabled us to make the first flint tools, a key step in the evolution of our species. In autistic disorders, there is a defect in the connection of short U-shaped white matter fibers linking this lobe withot her brain regions, as shown by a Neurospin team in 2018. The dysfunction of the short-distance connectome would explain the deficit in social cognition in autistic patients [7].
A fundamental aspect of the human species is the need for social cooperation, right from birth. This ability to cooperate and exchange knowledge has enabled us to survive against predators in the wild. It is now possible to study social cognition using 2-brain recording methods (hyper-scanning). The first studies of interactions between an ASDs child and an adult should soon be available [14–19].
Is it possible to detect autism spectrum disorder in the fetus before birth? / Можно ли выявить расстройство аутистического спектра у плода до рождения?
If the answer is yes, autism spectrum disorders may be associated with abnormal embryonic organogenesis, causing postnatal malformations in some autistic children. The second important point is that early detection and early intervention can improve the long-term course of autism.
Prenatal ultrasound can show early signs of later autism spectrum disorder. An Israeli study in 2022 reviewed the fetal ultrasound records of children later diagnosed with autism. A number of antenatal ultrasound anomalies were associated with a higher risk of autism. This was more frequent in girls than in boys. These signs varied, and included urinary tract pyelectasis, intracardiac echogenic zones and ventricular septal defects. In the brain, choroid plexus cysts, ventricular enlargement and mega-cisterns were noted, suggesting abnormal development of cerebrospinal fluid circulation. There could also be a small head circumference and an enlarged interocular distance [20].
It is now possible to study the functional connectome of the fetus in the 2nd trimester of pregnancy thanks to functional magnetic resonance imaging (fMRI). In 2019, a study published by the obstetrics team at Utrecht University explored 105 pregnant women in fMRI between 20 and 40 weeks' amenorrhea. The results are surprising. They show a similarity between the fetal connectome and the adult connectome in 61 % of cases. These results indicate that the fetal brain has a functional connectome that is close to that of an adult as early as the 2nd trimester of pregnancy. Fetal fMRI should enable us to better understand the development of the functional brain connectome, and thus detect NDDs [21].
Is it possible to detect autism spectrum disorders in infants after birth and before the age of 24 months? / Можно ли обнаружить расстройства аутистического спектра у младенцев после рождения и до 24-месячного возраста?
The clinical signs of autism typically begin in children in the second year of life. The majority of children are diagnosed around the age of four. Early identification of ASD would enable these children to benefit from early educational interventions at a time when there is greater brain plasticity between birth and age 4. This could be of great benefit to them. They could benefit greatly. Early biomarkers should tell healthcare teams which children to target for early intervention, and offer these children personalized treatment strategies.
The electroencephalogram (EEG) appears to be an interesting technique for the early diagnosis of autism from the age of three months in babies at high risk of the condition. A study by the Boston Children Hospital team published in 2018 showed that it was possible, using an artificial intelligence algorithm, to identify early differences in the complexity of the EEG signal. These differences were most pronounced in the frontal lobes in the delta bands. This method enabled a predictive diagnosis at nine months of age close to 100 % [22].
Another fMRI study, this time in babies at high risk of autism, carried out at six months of age, predicted the diagnosis of autism at 24 months. Functional MRI, coupled with an artificial intelligence algorithm, was able to detect which connections differed between children with and without autism, at the age of six months, an age when there are no behavioral signs suggestive of autism. The machine was able to correctly diagnose 9 of the 11 children who went on to develop autism. It made no mistakes in identifying children who did not have autism. However, the machine did not indicate which brain regions or connections were altered, and gave no indication of the biology underlying ASDs [23].
These methods, which use the study of the default mode of the baby's brain, i.e. spontaneous brain connections when the child is doing nothing in particular, look promising. Indeed, such biomarkers could tell us which children to target for early therapeutic intervention, and reveal the errors in fetal and infant brain development that lead to autism [24].
Anatomical MRI is also of interest in the diagnosis of autism by measuring increased cerebrospinal fluid in children who later develop autism. A 2017 study explored 221 children at high risk of autism using MRI coupled with a deep learning algorithm at ages 6, 12 and 24 months. An increase in extra-axial cerebrospinal fluid was detectable at six months of age in these children. This increase was associated with greater sleep disturbance and diminished verbal skills. This sign could be an interesting biomarker [25].
The availability to doctors and researchers of an atlas of cortical sulcus development and an atlas describing the multiple variations of the short-distance connectome by the Neurospin teams are already helping to identify cerebral markers of ASDs. For example, the maximum depth of a sulcus located in Broca's area, an area of articulated language and communication, is less in ASDs children. These new spatio-temporal models of cortical development should provide clinicians with valuable brain biomarkers [26–29].
Opening our eyes to autism / Откроем глаза на аутизм
Pupillary motricity and oculomotricity seem to be interesting diagnostic methods in high-risk children. Indeed, children who go on to develop autism have an increased pupillary reflex to light. Pupillary response is correlated with the severity of social symptoms. This change in reflexes may reflect an early abnormality in the child's cerebral development, but it may also be the emergence of atypical sensory processes that precede the onset of later behavioral symptoms. From as early as two months of age, there are also abnormalities in eye-tracking, including anomalies in the facial recognition process. Children who later develop profound autism show a decrease in ocular fixation between the first 2 and 6 months of life [30][31].
What preventive measures are possible? / Какие меры профилактики возможны?
Since the studies carried out on children in Romanian orphanages in the 1970s, we have learned the importance of social relationships in babies. Indeed, orphans who remained in orphanages had 30 IQ points less than those placed in foster homes. The pivotal age for this intellectual loss is around two years of age. In fact, orphans who remained in orphanages had 30 IQ points less than those placed in foster homes. The pivotal age for this intellectual loss is around two years of age. We are also beginning to understand the deleterious effects of screens on babies. Babies exposed to screens from an early age show six times more delayed language acquisition than unexposed children. It also seems important to protect pregnant women, nursing mothers and their babies from certain chemical pollutants and endocrine disruptors. In addition, during pregnancy, the quality of the mother's diet influences the neurodevelopment of the fetus. Pregnant women who eat the healthiest diet have the best-developed babies. In fact, nutrients such as vitamin B9, iron, iodine, zinc and omega-3 fatty acids appear to play an essential role in the healthy development of the fetal brain and baby [32–36].
What to do next? / Что делать дальше?
It's important to use non-stigmatizing language and methods for parents. In fact, the methods presented in certain articles are in the field of research, and the significant emotional charge associated with an autism diagnosis must be taken into account. Misdiagnosis is very difficult for parents. We propose a universal method of education, suitable for all children and starting at birth. It's important to know how to use the fantastic learning capacities of the baby's brain during the 1st wave of neuroplasticity from birth to age five. According to neuroscientist Stanislas Dehaene, who heads the Neurospin center: "Computers and artificial intelligence are no match for a newborn baby, the absolute model in terms of learning" [37–39].
"Developmental cocooning" / «Кокон развития»
This is a care program that begins at birth. This program extends from birth to the age of three, making the most of the baby's great neuroplasticity. It is an educational and screening program for parents and early childhood professionals, focusing on social and sensory interactions. The idea of this program is to act without waiting for a diagnosis of autism, in order to reduce the severity of the disease. Current programs start at the age of three and beyond. The idea of this program is to build as best we can the first row of stones on which we are all built. Indeed, the ingredients for a baby's brain develop mentare: loving parents, successful breastfeeding, an environment rich in stimulation, a ban on screens, and a diet rich in vitamin B9, omega-3 fatty acids, iron, iodine and zinc [40][41].
Discussion / Обсуждение
MRI and EEG methods coupled with artificial intelligence do not effectively predict autism severity in at-risk children. Nor do polygenic genetic scores. What's more, these technologies are not available on a routine clinical basis. They raise important ethical questions. However, a child's quality of life depends on the interventions he or she receives and how early they are implemented. The search for autoimmune diseases in pregnant women, which often go undetected, should enable us to learn more about one of the causes of cerebral neuroinflammation in the fetus, and a possible cause of ASDs [42].
These discoveries concerning the genetic component of autism are not purely descriptive, they also open up new therapeutic perspectives and the possibility of precision medicine. The genetic diagnosis of autism is no longer a measured finding. We are now in a position to propose a personalized care strategy. Understanding the genetic basis of autism has paved the way for an approach based on individual genetic diagnosis. In certain cases, this diagnosis can lead to personalized therapeutic adaptations. For example, in people with Smith-Magenis syndrome, a genetic disorder caused by a microdeletion of chromosome 17, it is beneficial, in order to restore the sleep-wake cycle of melatonin secretion, to prescribe melatonin in the evening and beta-blockers which inhibit melatonin secretion during the day. This treatment will enable people to get better and resume their social and professional lives. In some cases of ASDs children with intestinal microbiota disturbances, fecal transplants have been successfully tested. Other syndromes will benefit from a different treatment, meaning that diagnosis is now beginning to change the way we treat them. Identifying genes also enables us to detect metabolic diseases such as phenylketonuria, which are at the root of autism. This metabolic disease leads to an accumulation of phenylalanine in the body, which is toxic to the child's developing brain and causes intellectual impairment. It is then possible to modify the child's diet so that he or she does not suffer from intellectual deficiency. Clinical studies are underway to assess the efficacy of lithium on people with a Shank 3 gene mutation. In certain forms of autism with intellectual disability and/or epileptic seizures, forms of gene therapy may be possible in the future. The brain is a highly complex organ, and a great deal of research is still needed to develop these therapies [43][44].
The discovery of biomarkers for autism should revolutionize the diagnosis of ASDs based on the current clinical classification, and make it possible to establish precision diagnoses for each patient. This new biological classification will make it possible to differentiate between genetic, environmental and mixed forms. This process is already underway in oncology, where the current classification of tumors based on anatomy and organ location is gradually being replaced by biological classification, with some innovative treatments being proposed according to the genetic profile of tumors rather than their location. Precision treatment of ASDs will then be possible, tailored to the biological profile of each patient [45].
Conclusion / Заключение
Sophisticated imaging methods coupled with artificial intelligence algorithms make it possible to diagnose autism in infants before the age of 24 months. A combination of measurements in a child offers a better prediction of diagnosis than a single measurement. The care methods applied to babies from birth onwards require an efficient and competent human presence. It is important to trace the early development of autism at several levels of analysis: clinical, genetic, cerebral, behavioral and child health. If these screening methods are to become usable in clinical practice, they must be combined with beneficial interventions in children, and help to improve the quality of life of individuals diagnosed with autism. Our future studies must answer the questions asked by parents of babies at high risk of autism, and more generally by all parents:
– Will their child be autistic or not?
– Will their child have a severe form of autism or not?
– Will their child be independent in later life?
References
1. Dawson G., Rieder A.D., Johnson M.H. Prediction of autism in infants: Progress and challenges. Lancet Neurol. 2023;22(3):244-54. https://doi.org/10.1016/S1474-4422(22)00407-0.
2. Bourgeron T. Des genes, des synapses, des autismes. Paris: Odile Jacob, 2023. 320 p.
3. Warrier V., Zhang X., Reed P. et al. Genetic correlates of phenotypic heterogeneity in autism. Nat Genet. 2022;54(9):1293-304. https://doi.org/10.1038/s41588-022-01072-5.
4. Girault J., Donovan K., Hawsk Z. et al. Infant visual brain development and inherited genetic liability in autism. Am J Psychiatry. 2022;179(8):573-85. https://doi.org/10.1176/appi.ajp.21101002.
5. Magee J.C., Grienberger C. Synaptic plasticity forms and functions. Annu Rev Neurosci. 2020;43:95-117. https://doi.org/10.1146/annurev-neuro-090919-022842.
6. Tang G., Gudsnuk K., Kuo S.-H. et al. Loss of mTOR-dependent 2014;83(5):1131-43. https://doi.org/10.1016/j.neuron.2014.07.040.
7. D'Albis M.-A., Guevara P., Guevara M. et al. Local structural connectivity is associated with social cognition in autism spectrum disorder. Brain. 2018;141(12):3472-81. https://doi.org/10.1093/brain/awy275.
8. Caporale N., Leemans M., Birgersson L. et al. From cohorts to molecules: Adverse impacts of endocrine disrupting mixtures. Science. 2022;375(6582):eabe8244. https://doi.org/10.1126/science.abe8244.
9. Bongaerts E., Lecante LL., Bove H. et al. Maternal exposure to ambient black carbon particles and their presence in maternal and fetal circulation and organs: an analysis of two independent population-based observational studies. Lancet Planet Health. 2022;6(10):e804-e811. https://doi.org/10.1016/S2542-5196(22)00200-5.
10. Demeneix B. Cocktail toxique: Comment les perturbateurs endocriniens empoisonnent notre cerveau. Paris, Odile Jacob, 2017. 289 p.
11. Ahrens A.P., Hyotylainen T., Petrone J.R. et al. Infant microbes and metabolites point to childhood neurodevelopemental disorders. Cell. 2024;187(8):1853-1873.e15. https://doi.Org/10.1016/j.cell.2024.02.035.
12. Kang D.-W., Adams J.B., Coleman D.M. et al. Long-term benefit of Microbiota Transfer Therapy on autism symptoms and gut microbiota. Sci Rep. 2019;9(1):5821. https://doi.org/10.1038/s41598-019-42183-0.
13. Elandaloussi Y., Floris D.L., Coupe P et al. Understanding the relationshipbetweencerebellar structure and social habilities. MolAutism. 2023;14(1):18. https://doi.org/10.1186/s13229-023-00551-8.
14. Dumas G., Nadel J., Soussignan R. et al. Inter-brain synchronization during social interaction. Plos One. 2010;5(8):e12166. https://doi.org/10.1371/journal.pone.0012166.
15. Endevelt-Shapira Y., Djalovski A., Dumas G., Feldman R. Maternal chemosignals enhance infant-adult-brain-to-brain synchrony. Sci Adv. 2021;7(50):eabg6867. https://doi.org/10.1126/sciadv.abg6867.
16. Eggebrecht A., Elison J.T., Feczko E. et al. Joint attention and brain functional connectivity in infants and toddlers. Cereb Cortex. 2017;27(3):1709—20. https://doi.org/10.1093/cercor/bhw40.
17. Santamaria L., Noreika V., Georgieva S. et al. Emotional valence modulates the topology of the parent-infant inter-brain network. Neuroimage. 2020;207:116341. https://doi.org/10.1016/j.neuroimage.2019.116341.
18. Piazza P., Hazenfratz L., Hasson U., Lew-Williams C.L. Infant and adult brains are coupled to the dynamics of natural communication. Psychol Sci. 2020;31(1):6-17. https://doi.org/10.1177/0956797619878698.
19. Wang Q., Han Z., Hu X. et al. Autism symptoms modulate interpersonal neural synchronization in children with autism spectrum disorder in cooperative interactions. Brain Topography. 2020;33:112-22.
20. Regev O., Hadar A., Meiri G. et al. Association between ultrasonography fetal anomalies and autism spectrum disorder. Brain. 2022;145(12):4519- 30. https://doi.org/10.1093/brain/awac008.
21. Turk E., van Den Heuvel M., Benders M.J. et al. Functional connectome of the fetal brain. J Neuroscie. 2019;39(49):9716-24. https://doi.org/10.1523/JNEUROSCI.2891-18.2019.
22. Bosl W.J., Tager-Flusberg H., Nelson C.A. EEG analytics for early detection of autism spectrum disorder: A data-driven approach. Sci Rep. 2018;8(1):6828. https://doi.org/10.1038/s41598-018-24318-x.
23. Emerson R.W., Adams C., Nishino T. et al. Functional neuroimaging of high-risk 6-month-old infants predicts a diagnosis of autism at 24 months of age. Sci Translat Med. 2017;9(393):eaag2882. https://doi.org/10.1126/scitranslmed.aag2882.
24. Gao W., Zhu H., Giovanello K.S. et al. Evidence on the emergence of the brain's default network from 2-week-old to 2-year-old healthy pediatric subjects. Proc Natl Acad Sci U S A. 2009;106(16):6790-5. https://doi.org/10.1073/pnas.0811221106.
25. Shen M.D., Kim S.H., McKinstry R.C. et al. Increased extra-axial cerebrospinal fluid in high-risk infants who later develop autism. Biol Psychiatry. 2017;82(3):186-93. https://doi.org/10.1016/j.biopsych.2017.02.1095.
26. Leroy F., Mangin J.-F., Rousseau F. et al. Atlas-free surface reconstruction of the cortical grey-white matter interface in infants. PLoS One. 2011;6(11):e27128. https://doi.org/10.1371/journal.pone.0027128.
27. Guillon L., Chavas J., Benezit A. et al. Identification of rare cortical folding patterns using unsupervised deep learning. Imaging Neuroscience. 2024;2:1-27. https://doi.org/1./1162/imag_a_00084.
28. Mihailov A., Pron A., Lefevre J. et al. Normative models combining fetal and postnatal MRI data to characterize neurodevelopemental trajectories during transition from in- to ex-utero. bioRxiv. March 11, 2024. https://doi.org/10.1101/2024.03.07.583908.
29. Brun L., Auzias G., Viellard M. et al. Localized misfolding within Broca's area as a distinctive feature of autistic disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2016;1(2):160-8. https://doi.org/10.1016/j.bpsc.2015.11.003.
30. Nystrom P., Gliga T., Jobs E.N. et al. Enhanced pupillary reflex in in fancy is associated with autism diagnosis in toddlerhood. Nat Commun. 2018;9(1):1678. https://doi.org/10.1038/s41467-018-03985-4.
31. Guillon Q., Afzali M.H., Roge B. et al. The importance of networking in autisl gaze analysis. PLoS One. 2015;10(10):e0141191. https://doi.org/10.1371/journal.pone.0141191.
32. Katsantonis I., McLellan R. The role of parent-child interactions in the association between mental health and prosocial behavior: Evidence from early childhood to late adolescence. Int J Behav Dev. 2024;48(1):59-70. https://doi.org/10.1177/01650254231202444.
33. Collet M., Gagnaire B., Rousseau C. et al. L'exposition aux ecrans chez les jeunes enfants est-elle a l'origine de l'apparition de troubles primaires du langage ? Une etude cas-temoins en Ille et Villaine. BEH. 2020;1:17-27.
34. Hutton J., Dudley J., Horowitz-Kraus T. et al. Associations between screen-based media use and brain white matter integrity in preschool-ages children. JAMA Pediatr. 2020;174(1):e193869. https://doi.org/10.1001/jamapediatrics.2019.3869.
35. De Lauzon-Guillain B., Marques C., Kadawathagedara M. et al. Maternal diet during pregnancy and child neurodevelopment up to age 3.5 years: the nationwide Étude Longitudinale Française depuisl'Enfance (ELFE) birth cohort. Am J Clin Nutr. 2022;116(4):1101–11. https://doi.org/10.1093/ajcn/nqac206.
36. Guo A., Ludvigsson, Brantsaeter A.L. et al. Early-life diet and risk of inflammatory bowel disease: A pooled study in two Scandinavian birth cohorts. Gut. 2024;73(4):590-600. https://doi.org/10.1136/gutjnl-2023-330971.
37. Dehaene-Lambertz G., Spelke E. The infancy of the human brain. Neuron. 2015;88(1):93-109. https://doi.org/10.1016/j.neuron.2015.09.026.
38. Kouider S., Stalhut K., Gelskov S.V. A neural marker of perceptual consciousness in infants. Science. 2013;340(6130):376-80. https://doi.org/10.1126/science.1232509.
39. Dehaene S, Lau H, Kouider S. What is consciousness, and could machines have it? Science. 2017;358(6362):486-92. https://doi.org/10.1126/science.aan8871.
40. Cuillerier L., Genest C., Lefebvre H. Trouble du spectre de l'autisme: intervenir aupres de la clientele adolescente et de sa famille. Perspect Infirm. 2019;16(1):54-61.
41. Jeune M.A., Suarez B. Cocooning developpemental. Paris, Odile Jacob, 2025.
42. Green J., Charman T., Pickles A. et al.; BASIS team. Parent-mediated intervention versus no intervention for infants at high risk of autism: A parallel, single-blind, randomized trial. Lancet Psychiatry. 2015;2(2):133- 40. https://doi.org/10.1016/S2215-0366(14)00091-1.
43. Maruani A., Amsellem F., Tabet A.C. et al. Lithium et TSA. French Journal of Psychiatry. 2018;1:S45.
44. Ioannidis V., Pandey R., Bauer H.F. et al. Disrupted extracellular matrix and cell genes in autism-associated Shank 3 deficiency are targeted by lithium. Mol Psychiatry. 2023;29(3):704-17. https://doi.org/10.1038/s41380-023-02362-y.
45. Andre F., Rassy E., Marabelle A. et al. The waywename cancers needs to change. Nature. 2024;626(7997):26-9. https://doi.org/10.1038/d41586-024-00216-3
About the Authors
B. SuareFrance
Bruno Suarez, MD.
104 Boulevard Raymond Poincare, 92380 Garches
M.-A. Jeune
France
Marie-Agnes Jeune, MD.
12 rue Ernest Renan, 92310 Sevres
What is already known about this subject?
► The diagnosis of autism spectrum disorder (ASD) in children is based on clinical examination.
► Children are diagnosed around the age of 4.
What are the new findings?
► Using techniques such as magnetic resonance imaging and electroencephalography, it is possible to make early diagnoses as early as 6 months of age.
How might it impact on clinical practice in the foreseeable future?
► Early diagnosis of a child with an ASD could enable early therapeutic treatment.
► By taking advantage of the high degree of neuroplasticity in babies, the severity of the disease could be reduced.
Review
For citations:
Suare B., Jeune M. New perspectives on autism: two equations to describe a complex disorder and envisage new treatments. Obstetrics, Gynecology and Reproduction. 2024;18(6):882-890. https://doi.org/10.17749/2313-7347/ob.gyn.rep.2024.526

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.










































