Scroll to:
100 years of Moschcowitz disease and thrombotic microangiopathy research: a look into the past and prospects
https://doi.org/10.17749/2313-7347/ob.gyn.rep.2024.544
Abstract
In this article we review the history of the thrombotic microangiopathy (TMA) study over the past 100 years. Important events and discoveries made by scientists across the globe are described, which profoundly contributed to understanding TMA etiology, pathogenesis and treatment. The prospects for current TMA investigation especially in obstetric practice are discussed.
Keywords
For citations:
Shatilina A.Yu., Hajiyeva A.B., Valikhanova L.M., Meshcheryakov A.A., Gashimova N.R., Grigoreva K.N., Vorobev A.V. 100 years of Moschcowitz disease and thrombotic microangiopathy research: a look into the past and prospects. Obstetrics, Gynecology and Reproduction. 2024;18(4):603-611. https://doi.org/10.17749/2313-7347/ob.gyn.rep.2024.544
Introduction / Введение
Moschcowitz disease, commonly known as thrombotic thrombocytopenic purpura (TTP), has long remained a subject of in-depth research. Since its discovery in the first quarter of the twentieth century, the pathology, which is characterized by abnormalities in the blood coagulation system, has been the basis for numerous research studies aimed at gaining deeper insights into the biological nature and pathogenesis of the disease, thereby contributing to improving its diagnostics and treatment. The characteristic features of this pathology are microangiopathic hemolytic anemia (MAHA), thrombocytopenia and multiple organ dysfunction, now united under the term thrombotic microangiopathy (TMA). TMA comprises a group of diseases united by a common pathophysiological process characterized by arteriolar and capillary thrombosis. This results in damage to small blood vessels leading to red blood cell destruction due to passage through damaged vessels, decreased count of platelets actively consumed for clot formation, and multi-organ failure due to vascular thrombosis and impaired organ perfusion. Thrombotic microangiopathies include TTP, hemolytic uremic syndrome (HUS) as well as several secondary TMAs that may be caused by drug therapy, infections or comorbidities. Treatment options depend on the specific disease within the TMA group and may include plasmapheresis, immunosuppressive therapy, supportive care and, in the case of HUS, hemodialysis. It is important to note that regardless of the specific diagnosis, any nosology within the TMA group requires immediate medical intervention as it may turn into a life-threatening condition.
Discovery of Moshkovitz's disease / Открытие болезни Мошковица
Exactly one hundred years ago, in 1924, Dr. Eli Moschcowitz (Fig. 1) published the first description of a young female patient who died of a then-unknown acute illness. In 1924, a 16-year-old adolescent was admitted to Beth Israel Hospital in New York City with an acute illness. The patient complained of fever, pallor, petechiae, weakness and paralysis developing inleft arm and leg. She fell into coma and died one week after admission to the hospital [1]. Autopsy revealed widespread "hyaline" microthrombi in the capillaries and arterioles of various organs including the heart, spleen, and kidneys. The cause of this fatal disease in a seemingly healthy girl was unknown.

Figure 1. Eli Moschcowitz (1879–1964).
Рисунок 1. Эли Мошковиц (1879–1964).
In 1947, К. Singer et al. described a case of a girl whose autopsy findings were almost identical to those of Moschcowitz's patient: multiple microthrombi in various organs [2]. Before death, the girl had severe anemia with reticulocytosis and marked thrombocytopenia. К. Singer et al. proposed the hypothesis that microvascular thrombi were composed of platelets and fibrin, and after analyzing all patients with similar features reported at that time, they suggested that this is a specific disease in which thrombocytopenia results from massive intravascular platelet consumption in a disseminated microvascular thrombotic process. In contrast to the more common "idiopathic thrombotic thrombocytopenic purpura" (now known as immune thrombocytopenia), К. Singer proposed to call the disease "thrombotic thrombocytopenic purpura" [2]. This name is still used today.
In 1966, all patients registered at that time with TTP diagnosis were reviewed by E.L. Amorosi and J.E. Ultmann (Fig. 2) [3] and devised a diagnostic pentad of features: hemolytic anemia with morphological signs of erythrocyte fragmentation in the blood smear (schistocytes, helmet cells), consumption thrombocytopenia, neurological symptoms, renal dysfunction and fever. They also noted postmortem findings of widespread microvascular thrombosis without inflammatory blood vessel changes. The authors questioned the nature of "hyaline" microthrombi and noted that fatal outcome was observed in almost all patients, as well as separately underlined the lack of any effect of therapy [3].
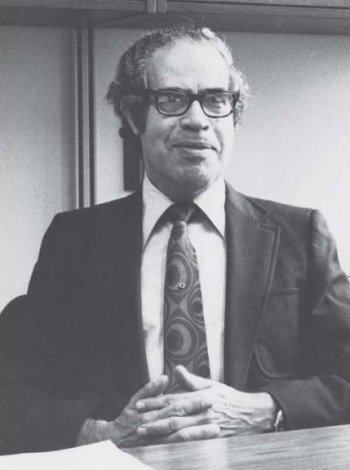
Figure 2. John Ernest Ultmann (1925–2000).
Рисунок 2. Джон Эрнест Ультманн (1925–2000).
von Willebrand factor discovery / Открытие фактора фон Виллебранда
In 1926, Dr. Eric von Willebrand (Fig. 3) described a hereditary coagulopathy now known as von Willebrand disease [4][5]. He observed a family in which patients with normal platelet counts died at different ages from hemorrhages of various genesis. In the 1950s and 1960s, a reduced level of factor VIII (FVIII) activity was identified as a plausible cause of this disease. It was also noted that the FVIII deficiency could be compensated by infusion of plasma or its individual fractions. Later, in 1971, an immunological analysis was performed, which revealed that hereditary coagulopathy was not caused by FVIII deficiency, but rather by an absolutely different protein, which was named after the discoverer – von Willebrand factor (vWF).
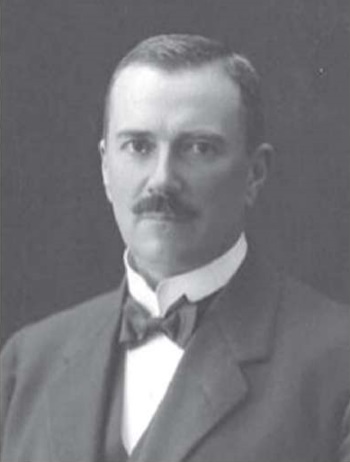
Figure 3. Erik Adolf von Willebrand (1870–1949).
Рисунок 3. Эрик Адольф фон Виллебранд (1870–1949).
Study of other forms of thrombotic microangiopathy / Изучение других форм тромботической микроангиопатии
In 1978, J.D. Upshaw (Fig. 4) published a case report in the New England Journal of Medicine [6] describing a 29-year-old woman who presented with recurrent episodes of fever, petechiae, marked thrombocytopenia and microangiopathic hemolytic anemia since the age of 6 months. Corticosteroid therapy, antibiotic therapy and splenectomy failed. However, blood transfusion led to improved patient's condition. J.D. Upshaw concluded that the plasma factor might be important, so that upon the next disease episode the patient was treated solely with two units of platelet-poor plasma. The patient responded well to infusion of fresh frozen plasma that normalized platelet count and hematocrit without a need for red blood cell transfusion.
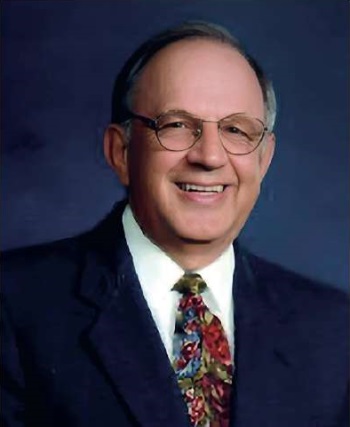
Figure 4. Jefferson D. Upshaw (1905–1983).
Рисунок 4. Джефферсон Д. Апшоу (1905–1983).
In 1955, under the leadership of C. Gasser, there was described a condition found in five children characterized by acute renal failure, hemolytic anemia and thrombocytopenia, which developed after infectious diarrhea due to Shiga toxin-producing Escherichia coli-HUS (STEC-HUS), they called this complex of symptoms HUS [7]. In 1966, HUS was described in detail by C. Gasser, so it is also called a Gasser’s disease [8]. HUS is characterized by a triad of symptoms: MAHA, thrombocytopenia and acute renal failure, affecting young children more often than adults. Inciting causes of HUS can include hemorrhagic colitis, malignancy and antitumor treatment, pregnancy, and organ transplantation. Since the pathogenetic link between HUS and verotoxin-producing Escherichia coli (VTEC) infection was noted in 1983, a marked advance in understanding VTEC infection as one of the leading HUS causes has been made [9].
Discovery of ADAMTS-13 and its role in hemostasis / Открытие ADAMTS-13 и ее роли в системе гемостаза
In 1982, J.L. Moak et al. (Fig. 5) described ultra-large vWF multimers in patients with chronic recurrent TTP [10]. Being the most thrombogenic vWF counterpart, they were released from Weibel–Palade bodies [11] and entered the bloodstream upon stimulation or damage to vascular endothelial cells [12]. J.L. Moak et al. suggested that such multimers present in plasma during remission were responsible for platelet aggregation and adhesion in the microvascular bed during acute TTP episodes, as they disappeared from the plasma at this time. The existence of such hyper-adhesive molecules was thought to be due to a deficiency of vWF "depolymerase", which is characteristic of TTP. Ultra-large vWF multimers are converted into smaller and less thrombogenic multimers by a vWF-cleaving protease. In 1996, two research groups independently reported a novel metalloprotease isolated from human plasma that specifically cleaves vWF [13][14].
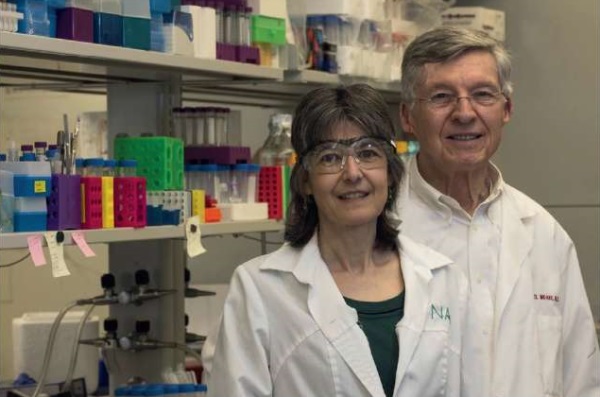
Figure 5. Joel Moake and Nancy Turner.
Рисунок 5. Джоэль Моак и Нэнси Тернер.
A year later, M. Furlan et al. published the study with four patients suffering from familial chronic recurrent TTP: two brothers with elevated plasma vWF multimer levels and a complete deficiency in the activity of the protease that cleaves vWF, as well as their parents without disease symptoms, with activity of this protease reduced to about half of normal. None of these patients had any plasma inhibitor or antibody against vWF-cleaving protease. They also noted that the ultra-large vWF multimers found in patients were related to insufficient activity of the protease that cleaves vWF. Deficiency of this protease may be inherited in an autosomal recessive manner and appears to predispose to chronic TTP recurrence. Analyzing vWF-cleavage protease activity can be used as a sensitive diagnostic tool to identify subjects with an underlying tendency to TTP [15].
In 2001, three research groups successfully purified the vWF-cleaving protease to a homogeneous state, which allowed to study its amino acid sequence [16–18]. Based on this, Х. Zheng et al. (Fig. 6) identified the vWF-cleaving protease as a new ADAMTS family member designated as ADAMTS-13 (a disintegrin and metalloprotease with thrombospondin type 1 motif, member 13) [19]. ADAMTS-13 deficiency can be caused by genetic mutations [6] or acquired factors such as the action of anti-ADAMTS-13 inhibitors [20][21] and/or its consumption due to sepsis [22], preeclampsia, cancer, antiphospholipid syndrome (APS). More recently, B. Plaimauer et al. expressed functionally active recombinant ADAMTS-13 in mammalian cells [23], which when added to the plasma from a patient with hereditary TTP compensated for the protease deficiency of vWF cleavage [24]. Thus, ADAMTS-13 turned out to be the missing plasma factor in the patient with congenital TTP noted above by J.D. Upshaw.

Figure 6. Xi Long Zheng.
Рисунок 6. Си Лонг Чжэн.
Until the 1970s, TTP was almost always fatal [3]. In 1959, М.А. Rubinstein et al. described a case of unexpected remission in a patient with TTP treated with fresh whole blood infusion [25]. In the following years, several cases were published on the beneficial effects of exchange transfusion of whole blood, plasmapheresis with fresh frozen plasma replacement or large volume plasma infusions [26]. This was carried out in order to provide sufficient ADAMTS-13. In 1991, an important randomized controlled trial was published by G.A. Rock et al. on behalf of the Canadian Apheresis Study Group, which unequivocally established the superiority of plasma replacement over simple plasma infusion in terms of response rate [27]. The rationale for this is the removal of autoantibodies with plasma replacement, which is not observed with simple plasma infusion. Among other drugs, corticosteroids have also been used in less severe cases, sometimes even excluding plasmapheresis [28]. The essence of therapy is to inhibit autoantibody production. In extreme cases, splenectomy was performed, thereby removing autoantibody-producing lymphocytes.
Role of thrombotic microangiopathy in obstetric practice / Роль тромботической микроангиопатии в акушерской практике
TTP in pregnancy was first described in 1955 by P.F. Miner et al., who noted that it is characterized by rapid progression of the disease with poor survival of both mother and fetus. The strategy for TTP treatment during pregnancy include the use of corticosteroids, antiaggregants, splenectomy, exchange plasmapheresis, exchange blood transfusion and plasma infusion, which allows not only to achieve remission, but also to prolong pregnancy [29].
In Russia, the analysis of thrombotic microangiopathy in pregnant women was first described in 2013 in the article prepared at the Department of Obstetrics and Gynecology of Sechenov University supervised by Academician A.D. Makatsariya that outlined the issues of pathogenesis and prevention of complications of pregnancy caused by TMA [30]. It was found out that pregnancy per se is a trigger for developing TMA. It is caused by dysadaptive changes in the hemostasis system during pregnancy, during which TMA can develop as TTP, HUS, heparin-induced thrombocytopenia (HIT) and HELLP syndrome. The discovery of TMA molecular mechanisms provides an alternative view on the pathogenesis of placenta-associated obstetric complications, including severe preeclampsia.
This idea was continued in the article prepared in 2014, in which the issues of preeclampsia and HELLP syndrome as a TMA manifestation were outlined and analyzed additionally describing the pathogenesis, diagnostics, and principles of therapy. The possibility for physiologically increased vWF levels characteristic of pregnancy, active uptake and depletion of ADAMTS-13 depots, which may exacerbate the previously latent deficiency of this enzyme, has been discussed. It was outlined that such mechanisms may play a role in severe placenta-associated complications of pregnancy [31].
In 2017, an in-depth analysis of TMA issue in pregnant women allowed to prepare for the first time a monograph in Russian "Thrombotic microangiopathies in obstetric practice" edited by Academician A.D. Makatsariya (Fig. 7), which outlined the etiology, pathogenesis, clinical picture, diagnostics and differential diagnosis, as well as modern principles for TMA prevention and treatment in obstetric practice. The pathogenesis of thrombotic microangiopathy due to hereditary and acquired ADAMTS-13 metalloprotease deficiency is described. A potential role of ADAMTS-13 deficiency in the pathogenesis of severe preeclampsia and catastrophic forms of antiphospholipid syndrome is discussed [32].
Figure 7. Monograph «Thrombotic microangiopathy in obstetric practice».
Рисунок 7. Монография «Тромботические микроангиопатии в акушерской практике».
Thrombotic microangiopathy in cancer patients / Тромботическая микроангиопатия у онкологических больных
In recent years, the number of studies investigating the TMA features in cancer patients has increased dramatically. Mechanisms contributing to TMA development are considered as the elements of the hemostasis system, which alter its functioning (chronic DIC syndrome) that accounts for a high incidence of thrombotic complications, development of multi-organ failure, and, consequently, associated high mortality.
The issue of studying thrombotic microangiopathy in cancer patients dates back to the work by K.H. Antman, who suggested in 1979 in the review on cancer-related MAHA that hemolysis and thrombocytopenia were caused mainly by mechanical obstruction of the vascular lumen by tumor emboli [33]. Later, it was found that cancer patients vs. general population had elevated blood vWF levels and, conversely, lower ADAMTS-13 levels, so that this difference often deteriorates with cancer progression [34].
In malignant neoplasms, changes in the ADAMTS-13/vWF ratio may result from excessive metalloprotease consumption due to upregulated vWF expression by activated endothelium. In conditions of absolute or relative (in the presence of antibodies) ADAMTS-13 deficiency, this may further activate platelet aggregation and the formation of tumor-platelet emboli. The mechanisms underlying development of absolute or relative ADAMTS-13 deficiency are still poorly understood, but studies conducted at the Department of Obstetrics and Gynecology of Sechenov University supervised by Academician A.D. Makatsariya are devoted to clarify it [35].
Prospects for studying thrombotic microangiopathy / Перспективы изучения тромботической микроангиопатии
Current treatment methods for TMA especially congenital TTP are ineffective and extremely inconvenient, because such patients require either lifelong ADAMTS-13 administration, which has a strong negative impact on the patients’ quality of life or lifelong treatment with plasma preparations every 1–3 weeks, which brings various health risks such as the development of allergic reactions, regular invasive procedures, as well as frequent hospital visits that greatly interfere with the daily life of patients [36–39]. The use of recombinant human ADAMTS-13 (rADAMTS-13) may be a promising alternative for patients with congenital TTP [40]. The efficacy of prophylactic rADAMTS-13 use in such patients has been demonstrated in pilot clinical trials. ADAMTS-13 activity reached approximately normal levels and adverse events were generally mild to moderate in severity, whereas TTP clinical manifestations were rare [41]. The clinical use of rADAMTS-13 was also reported, which resulted in a rapid effect in a 27-year-old patient with severe obstetric complications and a history of arterial thrombosis, who was diagnosed with hereditary TTP due to severe ADAMTS-13 deficiency [42]. However, the potential benefits, efficacy and safety of rADAMTS-13 use in patients with immune TTP remain incompletely understood. The ability of rADAMTS-13 to form immune complexes with autoantibodies, thereby promoting their clearance, has also been noted [43].
Also, gene therapy aimed at enhancing endogenous ADAMTS-13 expression may be a promising option for the treatment of congenital TTP. Studies in mice have shown that gene therapy for congenital TTP is feasible, but more preclinical animal studies are still needed to demonstrate the safety of this approach. Viral and non-viral vector systems using a liver-specific promoter that targets long-term ADAMTS-13 expression without inducing antibody response against ADAMTS-13 and without genotoxicity are considered as potential gene therapies for congenital TTP [44].
Conclusion / Заключение
Over the past 100 years, a prominent progress has been made in the diagnostics, treatment, and most importantly prevention of thrombotic thrombocytopenic purpura. Modern understanding of the disease pathophysiology has been the foundation for developing new approaches and methods for patient management. Today, TTP treatment no longer faces major obstacles, especially when it comes to early detection as well as timely therapy initiation. However, despite significant advances, it seems particularly important to further investigate the pathophysiological mechanisms underlying the vWF/ADAMTS-13 axis in order to prevent relapses.
In summary, over the last century, notable advances have been made in the field of TMA research, contributing to deeper understanding of the disease pathophysiology and subsequent development of novel diagnostic and therapeutic approaches. Not least among them, is equally to continue to move forward by gaining deeper insights and finding new solutions.
References
1. Moschcowitz E. Hyaline thrombosis of the terminal arterioles and capillaries: a hitherto undescribed disease. Proc NY Pathol Soc. 1924;24:21-4.
2. Singer K., Bornstein F.P., Wile S.A. Thrombotic thrombocytopenic purpura; hemorrhagic diathesis with generalized platelet thromboses. Blood. 1947;2(6):542-54.
3. Amorosi E.L., Ultmann J.E. Thrombotic thrombocytopenic purpura: report of 16 cases and review of the literature. Medicine (Baltimore). 1966;45(02):139-60.
4. Von Willebrand E.A. Hereditar pseudohemofili. Finska Lakarsallskapets Handl. 1926;67:7-112. (In Swedish).
5. Thachil J., Lassila R. What can historical literature on von Willebrand disease teach us? Res Pract Thromb Haemost. 2023;7(8):102244. https://doi.org/10.1016/j.rpth.2023.102244.
6. Upshaw J.D. Congenital deficiency of a factor in normal plasma that reverses microangiopathic hemolysis and thrombocytopenia. N Engl J Med. 1978;298(24):1350-2.
7. Gasser C., Gautier E., Steck A. et al. Hemolytic-uremic syndrome: bilateral necrosis of the renal cortex in acute acquired hemolytic anemia. Schweiz Med Wochenschr. 1955;85(38-39):905-9. (In German).
8. Gasser C. The hemolytic-uremic syndrome. Ther Umsch. 1968;25(8):433-7. (In German).
9. Karmali M.A., Steele B.T., Petric M., Lim C. Sporadic cases of haemolytic-uraemic syndrome associated with faecal cytotoxin and cytotoxin-producing Escherichia coli in stools. Lancet. 1983;1(8325):619-20. https://doi.org/10.1016/s0140-6736(83)91795-6.
10. Moake J.L., Rudy C.K., Troll J.H. et al. Unusually large plasma factor VIII: von Willebrand factor multimers in chronic relapsing thrombotic thrombocytopenic purpura. N Engl J Med. 1982;307(23):1432-5. https://doi.org/10.1056/NEJM198212023072306.
11. Wagner D.D. The Weibel-Palade body: the storage granule for von Willebrand factor and P-selectin. Thromb Haemost. 1993;70(1):105-10.
12. Arya M., Anvari B., Romo G.M. et al. Ultralarge multimers of von Willebrand factor form spontaneous high-strength bonds with the platelet glycoprotein Ib-IX complex: studies using optical tweezers. Blood. 2002;99(11):3971-7. https://doi.org/10.1182/blood-2001-11-0060.
13. Furlan M., Robles B.L.B. Partial purification and characterization of a protease from human plasma cleaving von Willebrand factor to fragments produced by in vivo proteolysis. Blood. 1996;87(10):4223-34.
14. Tsai H.M. Physiologic cleavage of von Willebrand factor by a plasma protease is dependent on its conformation and requires calcium ion. Blood. 1996;87(10):4235-44. https://doi.org/10.1182/blood.v87.10.4235.blood-journal87104235.
15. Furlan M7., Robles R., Solenthaler M. et al. Deficient activity of von Willebrand factor-cleaving protease in chronic relapsing thrombotic thrombocytopenic purpura. Blood. 1997;89(9):3097-103.
16. Gerritsen H.E., Robles R., Lammle B., Furlan M. Partial amino acid sequence of purified von Willebrand factor-cleaving protease. Blood. 2001;98(6):1654-61. https://doi.org/10.1182/blood.v98.6.1654.
17. Soejima K., Mimura N., Hirashima M. et al. A novel human metalloprotease synthesized in the liver and secreted into the blood: possibly, the von Willebrand factor-cleaving protease? J Biochem. 2001;130(4):475-80. https://doi.org/10.1093/oxfordjournals.jbchem.a003009.
18. Fujikawa K., Suzuki H., McMullen B., Chung D. Purification of human von Willebrand factor-cleaving protease and its identification as a new member of the metalloproteinase family. Blood. 2001;98(6):1662-6. https://doi.org/10.1182/blood.v98.6.1662.
19. Zheng X., Chung D., Takayama T.K. et al. Structure of von Willebrand factor-cleaving protease (ADAMTS13), a metalloprotease involved in thrombotic thrombocytopenic purpura. J Biol Chem. 2001;276(44):41059-63. https://doi.org/10.1074/jbc.C100515200.
20. Tsai H.M., Lian E.C. Antibodies to von Willebrand factor-cleaving protease in acute thrombotic thrombocytopenic purpura. N Engl J Med. 1998;339(22):1585-94. https://doi.org/10.1056/NEJM199811263392203.
21. Furlan M., Robles R., Galbusera M. et al. von Willebrand factor-cleaving protease in thrombotic thrombocytopenic purpura and the hemolytic-uremic syndrome. N Engl J Med. 1998;339(22):1578-84. https://doi.org/10.1056/NEJM199811263392202.
22. Ono T., Mimuro J., Madoiwa S. et al. Severe secondary deficiency of von Willebrand factor-cleaving protease (ADAMTS13) in patients with sepsis-induced disseminated intravascular coagulation: its correlation with development of renal failure. Blood. 2006;107(2):528-34. https://doi.org/10.1182/blood-2005-03-1087.
23. Plaimauer B., Zimmermann K., Volkel D. et al. Cloning, expression, and functional characterization of the von Willebrand factor - cleaving protease (ADAMTS13). Blood. 2002;100(10):3626-32. https://doi.org/10.1182/blood-2002-05-1397.
24. Antoine G., Zimmermann K., Plaimauer B.et al. ADAMTS13 gene defects in two brothers with constitutional thrombotic thrombocytopenic purpura and normalization of von Willebrand factor-cleaving protease activity by recombinant human ADAMTS13. Br J Haematol. 2003;120(5):821-4. https://doi.org/10.1046/j.1365-2141.2003.04183.x.
25. Rubinstein M.A., Kagan B.M., MacGillviray M.H. et al. Unusual remission in a case of thrombotic thrombocytopenic purpura syndrome following fresh blood exchange transfusions. Ann Intern Med. 1959;51:1409-19. https://doi.org/10.7326/0003-4819-51-6-1409.
26. Shepard K.V., Bukowski R.M. The treatment of thrombotic thrombocytopenic purpura with exchange transfusions, plasma infusions, and plasma exchange. Semin Hematol. 1987;24(3): 178-93.
27. Rock G.A., Shumak K.H., Buskard N.A. et al.; Canadian Apheresis Study Group. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. N Engl J Med. 1991;325(6):393-7. https://doi.org/10.1056/NEJM199108083250604.
28. Bell W.R., Braine H.G., Ness P.M., Kickler T.S. Improved survival in thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Clinical experience in 108 patients. N Engl J Med. 1991;325(6):398-403. https://doi.org/10.1056/NEJM199108083250605.
29. Miner P.E., Nutt R.L., Thomas M.E. Thrombotic thrombocytopenic purpura occurring in pregnancy. Am J Obstet Gynecol. 1955;70(3):611-7. https://doi.org/10.1016/0002-9378(55)90355-0.
30. Makatsariya A.D., Bitsadze V.O., Akinshina S.V., Andreeva M.D. The pathogenesis and prevention of complications of pregnancy conditioned by thrombotic microangiopathy. [Patogenez i profilaktika oslozhnenij beremennosti, obuslovlennyh tromboticheskoj mikroangiopatiej]. Voprosy ginekologii, akusherstva i perinatologii. 2013;12(6):63-73. (In Russ.).
31. Makatsariya A.D., Akinshina S.V., Bitsadze V.O. Preeclampsia and HELLP syndrome as a manifestation of thrombotic microangiopathy. [Preeklampsiya i HELLP-sindrom kak proyavlenie tromboticheskoj mikroangiopatii]. Akusherstvo i ginekologiya. 2014;(4):4-10. (In Russ.).
32. Makatsariya A.D., Bitsadze V.O., Khirzoeva J.Kh., Akinshina S.V. Thrombotic microangiopathies in obstetric practice. [Tromboticheskie mikroangiopatii v akusherskoj praktike]. Moscow: GEOTAR-Media, 2017. 304 p. (In Russ.).
33. Antman K.H., Skarin A.T., Mayer R.J. et al. Microangiopathic hemolytic anemia and cancer: a review. Medicine. 1979;58(5):377-84. https://doi.org/10.1097/00005792-197909000-00004.
34. Terrell D.R., Williams L.A., Vesely S.K. et al. The incidence of thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: all patients, idiopathic patients, and patients with severe ADAMTS-13 deficiency. J Thromb Haemost. 2005;3(7):1432-6. https://doi.org/10.1111/j.1538-7836.2005.01436.x.
35. Makatsariya A.D., Elalami I., Vorobev A.V. et al. Thrombotic microangiopathy in cancer patients. [Tromboticheskaya mikroangiopatiya u onkologicheskih bol'nyh]. Vestnik RAMN. 2019;74(5):323-32. (In Russ.). https://doi.org/10.15690/vramn1204.
36. Deford C.C., Reese J.A., Schwartz L.H. et al. Multiple major morbidities and increased mortality during long-term follow-up after recovery from thrombotic thrombocytopenic purpura. Blood. 2013;122(12):2023-9. https://doi.org/10.1182/blood-2013-04-496752.
37. Falter T., Boschen S., Schepers M. et al. Influence of personality, resilience and life conditions on depression and anxiety in 104 patients having survived acute autoimmune thrombotic thrombocytopenic purpura. J Clin Med. 2021;10(2):365. https://doi.org/0.3390/jcm10020365.
38. Riva S., Mancini I., Maino A. et al. Long-term neuropsychological sequelae, emotional wellbeing and quality of life in patients with acquired thrombotic thrombocytopenic purpura. Haematologica. 2020;105(7):1957-62. https://doi.org/10.3324/haematol.2019.22642.
39. Westwood J.P., Scully M. Management of acquired, immune thrombocytopenic purpura (iTTP): beyond the acute phase. Ther Adv Hematol. 2022;13:20406207221112216. https://doi.org/10.1177/20406207221112217.
40. Woods A.I., Paiva J., Dos Santos C. et al. From the discovery of ADAMTS13 to current understanding of its role in health and disease. Semin Thromb Hemost. 2023;49(3):284-94. https://doi.org/10.1055/s-0042-1758059.
41. Scully M., Antun A., Cataland S.R. et al.; cTTP Phase 3 Study Investigators. Recombinant ADAMTS13 in congenital thrombotic thrombocytopenic purpura. N Engl J Med. 2024;390(17):1584-96. https://doi.org/10.1056/NEJMoa2314793.
42. Asmis L.M., Serra A., Krafft A. et al. Recombinant ADAMTS13 for hereditary thrombotic thrombocytopenic purpura. N Engl J Med. 2022;387(25):2356-61. https://doi.org/10.1056/NEJMoa2211113.
43. Bendapudi P.K., Foy B.H., Mueller S.B. et al. Recombinant ADAMTS13 for immune thrombotic thrombocytopenic purpura. N Engl J Med. 2024;390(18):1690-8. https://doi.org/10.1056/NEJMoa2402567.
44. Dekimpe C., Roose E., Sakai K. et al. Toward gene therapy for congenital thrombotic thrombocytopenic purpura. J Thromb Haemost. 2023;21(5):1090-9. https://doi.org/10.1016/j.jtha.2022.12.018.
About the Authors
A. Yu. ShatilinaRussian Federation
Anastasia Yu. Shatilina.
8 bldg. 2, Trubetskaya Str., Moscow 119991
A. B. Hajiyeva
Azerbaijan
Aygun B. Hajiyeva.
33 Huseyn Javid Avenue, Baku, AZ1143
L. M. Valikhanova
Azerbaijan
Lala M. Valikhanova.
33 Huseyn Javid Avenue, Baku, AZ1143
A. A. Meshcheryakov
Russian Federation
Arseniy A. Meshcheryakov.
4 Dolgorukovskaya Str., Moscow 127006
N. R. Gashimova
Russian Federation
Nilufar R. Gashimova - MD.
8 bldg. 2, Trubetskaya Str., Moscow 119991
K. N. Grigoreva
Russian Federation
Kristina N. Grigoreva - MD.
8 bldg. 2, Trubetskaya Str., Moscow 119991
A. V. Vorobev
Russian Federation
Alexander V. Vorobev - MD, PhD.
8 bldg. 2, Trubetskaya Str., Moscow 119991
Scopus Author ID 57191966265; Wos ResearcherID F-8804-2017
Review
For citations:
Shatilina A.Yu., Hajiyeva A.B., Valikhanova L.M., Meshcheryakov A.A., Gashimova N.R., Grigoreva K.N., Vorobev A.V. 100 years of Moschcowitz disease and thrombotic microangiopathy research: a look into the past and prospects. Obstetrics, Gynecology and Reproduction. 2024;18(4):603-611. https://doi.org/10.17749/2313-7347/ob.gyn.rep.2024.544

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.











































